Fentanyl Patch Heat Risk Calculator
How Heat Affects Your Patch
The article explains that even mild heat can increase fentanyl absorption by 33% at 40°C (104°F). This calculator estimates your risk based on your current temperature and activities.
People using fentanyl patches for chronic pain might think they’re safe as long as they follow the dosage schedule. But here’s the harsh truth: fentanyl patches can turn deadly if you get too warm-even slightly. It’s not just about heating pads or hot tubs. A fever, a warm room, even a long shower can push your body into an overdose you never saw coming.
How Fentanyl Patches Work (And Why Heat Changes Everything)
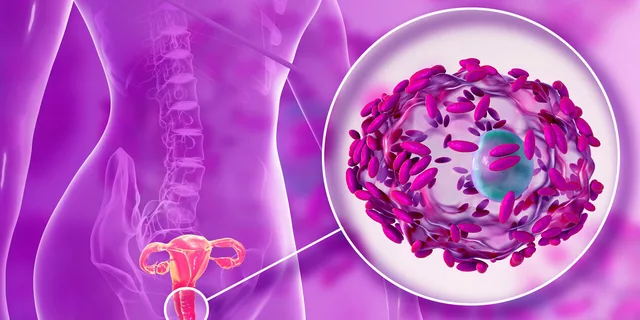
Fentanyl patches, like Duragesic, are designed to release the drug slowly through your skin over 72 hours. They’re not meant for quick relief. They’re for people with severe, ongoing pain who’ve already built up a tolerance to opioids. The patch holds a concentrated dose-sometimes enough to kill someone who’s never taken opioids before.
The drug doesn’t just leak out. It’s held in a gel layer, then moves through tiny pores in the patch, into your skin, and finally into your bloodstream. Your body’s blood flow and skin temperature control how fast it gets absorbed. Normally, this process is slow and steady. But heat? Heat breaks that control.
When your skin warms up, your blood vessels expand. More blood flows to the area under the patch. That means fentanyl gets pulled into your system faster. Studies show that if your body temperature hits 40°C (104°F), your fentanyl blood levels can jump by 33%. That’s not a small bump. That’s the difference between pain relief and stopped breathing.
Real Cases: Heat Turned a Patch Into a Death Trap
This isn’t theoretical. The Medical Letter documented three real cases where people overdosed because of heat:
- A man used a heating pad for back pain while wearing a fentanyl patch. He slipped into respiratory failure.
- A patient had surgery and was wrapped in a warming blanket. His fentanyl levels spiked. He stopped breathing.
- An elderly woman was active for a few hours, then collapsed. Her body heat from exertion accelerated fentanyl absorption.
In all three cases, the patients weren’t taking extra patches. They weren’t misusing the drug. They just got too warm. And their bodies absorbed too much, too fast.
What Counts as ‘Heat’? (It’s More Than You Think)
You might think only obvious heat sources matter. But the risks go way beyond that.
Here’s what you must avoid:
- Heating pads or electric blankets
- Saunas, steam rooms, hot tubs
- Long, hot showers or baths
- Sunbathing or tanning lamps
- Heated car seats or massage chairs with heat settings
- Wearing heavy clothing or layers in warm weather
- Strenuous exercise-even walking fast on a hot day
- Fever from infection (flu, pneumonia, UTIs)
Doctors at Mayo Clinic and the American Society of Anesthesiologists all say the same thing: Heat accelerates absorption. Always assume it’s dangerous.
Even something as simple as sitting near a radiator or sleeping under a thick duvet can raise your skin temperature enough to matter. And if you’re older, less active, or have poor circulation, your body might not regulate heat well-making you even more vulnerable.

What Happens After You Remove the Patch?
Many people think once they take the patch off, the danger’s over. It’s not.
Fentanyl stays in your skin and fat tissue for hours-even days-after removal. If you get hot during that time, your body can still absorb leftover drug. That’s why you’re told to fold the used patch in half (sticky sides together) and throw it out of reach of kids or pets. It’s not just about disposal. It’s about preventing accidental exposure while the drug is still leaving your body.
One study showed that even 24 hours after patch removal, fentanyl levels were still detectable-and rising if the person was exposed to heat.
Other Hidden Risks That Make It Worse
Heat isn’t the only problem. Some medications make it worse.
Drugs like ketoconazole (for fungal infections), erythromycin (an antibiotic), or certain antidepressants block the liver enzyme that breaks down fentanyl. If you’re taking one of these, your body can’t clear the drug fast enough. Add heat on top of that? You’re stacking risks.
Also, people with liver or kidney disease process fentanyl slower. That means even normal doses can build up. Heat pushes it over the edge.
And don’t forget: fentanyl patches are not for new opioid users. They’re not for post-surgery pain. They’re not for occasional use. The FDA warns they’re only for people who are already tolerant to opioids. A single patch can kill someone who’s never taken opioids before.

What to Do If You’re on a Fentanyl Patch
If you or someone you care for uses these patches, here’s what you need to do:
- Check your body temperature daily. If you have a fever, call your doctor. Don’t wait.
- Keep your environment cool. Use fans, not heaters. Wear light, breathable clothes.
- Avoid hot showers. Keep water lukewarm. No more than 10 minutes.
- Never use a heating pad, electric blanket, or sauna-even if you think it’s low heat.
- Ask your doctor about other meds you’re taking. Some can interact dangerously with fentanyl.
- Watch for signs of overdose: extreme drowsiness, slow or shallow breathing, cold/clammy skin, confusion, unresponsiveness.
- If you see these signs, call emergency services immediately. Naloxone can reverse it-but only if given fast.
Why This Keeps Happening
Doctors know the risks. But patients? Many don’t. The patch looks harmless. It’s small. It sticks to your skin like a bandage. People don’t realize it’s a concentrated opioid delivery system.
And the warnings? They’re buried in paperwork. Patients get the patch, read the small print, and forget. Or worse-they hear ‘slow release’ and assume it’s safe to ignore environmental factors.
But the science is clear. Heat doesn’t just increase absorption. It turns a controlled medical tool into a silent killer.
What’s Being Done?
Hospitals and pharmacies are starting to do better. Some now require patients to sign a safety checklist before getting a fentanyl patch. Others include heat warnings on the label in bold.
Researchers are exploring new patch designs that resist heat changes, but none are widely available yet. For now, the only reliable protection is awareness and discipline.
There’s no magic fix. No new technology that will make this safe without user responsibility. The patch works. But only if you treat it like the powerful, dangerous drug it is.
If you’re on a fentanyl patch, your safety doesn’t depend on the patch. It depends on you.
Can a fever cause a fentanyl overdose?
Yes. A fever raises your body temperature, which increases blood flow to the skin under the patch. This speeds up how fast fentanyl enters your bloodstream. Even a mild fever of 38.5°C (101.3°F) can raise drug levels enough to cause dangerous side effects like slowed breathing. If you develop a fever while using a fentanyl patch, contact your doctor immediately. Do not wait for symptoms to appear.
Is it safe to use a fentanyl patch if I have a cold or flu?
It’s not safe without medical guidance. Colds and flu often cause fever, which increases fentanyl absorption. Even without fever, your body is under stress, and your liver and kidneys may not process the drug as efficiently. Always tell your doctor if you’re sick before using or continuing a fentanyl patch. They may adjust your dose or suggest a different pain treatment.
Can I take a hot shower if I have a fentanyl patch?
No. Hot water raises your skin temperature and increases blood flow to the patch area. This can cause a sudden spike in fentanyl levels. Stick to lukewarm showers under 10 minutes. Avoid soaking in baths or using steam rooms. If you need to clean the area around the patch, gently pat it with a damp cloth instead.
What should I do if I accidentally expose my patch to heat?
If you’ve been near a heat source-like a heater, sunlamp, or hot car-watch for signs of overdose: dizziness, extreme sleepiness, slow breathing, or confusion. If you notice any of these, remove the patch immediately and call emergency services. Even if you feel fine, call your doctor. They may want to monitor your condition or adjust your next dose.
Can I use a heating pad on another part of my body while wearing a fentanyl patch?
No. Heat from any source can raise your overall body temperature, even if it’s not directly on the patch. Your blood circulates throughout your body, and even a small rise in temperature can increase fentanyl absorption. Never use a heating pad, electric blanket, or heated seat while wearing a fentanyl patch-even if it’s on your back and the patch is on your arm.
How long does fentanyl stay in my body after removing the patch?
Fentanyl can remain in your skin and fat tissue for up to 24-48 hours after removing the patch. During this time, your body is still absorbing the leftover drug. That’s why you must still avoid heat sources-even after taking the patch off. Do not use saunas, take hot showers, or exercise vigorously for at least two days after removal.




Chris Urdilas
January 28, 2026 AT 15:54So let me get this straight - you’re telling me my grandma’s 10-minute warm shower could kill her? And we just hand these patches out like Band-Aids? I mean, I get it’s for chronic pain, but if the FDA’s got to slap a warning label on it like it’s a radioactive banana, maybe we shouldn’t be giving it to people who can’t even turn on the AC without help.
Also, why isn’t this on the patch itself in neon letters? 'WARNING: DO NOT BREATHE, MOVE, OR EXIST NEAR A WINDOW ON A SUMMER DAY.'
People are dying because the system assumes they’re smart enough to read the tiny print. But most of them are 70 and blind as a bat. This isn’t a medical issue - it’s a design failure.
Jeffrey Carroll
January 28, 2026 AT 20:24It is imperative to recognize that fentanyl transdermal patches represent a class of pharmaceutical agents requiring stringent environmental and physiological monitoring. The pharmacokinetic profile of fentanyl is demonstrably sensitive to dermal temperature elevation, as evidenced by peer-reviewed clinical studies indicating a statistically significant increase in plasma concentration under hyperthermic conditions.
Healthcare providers must ensure that patients receive comprehensive, documented education regarding thermal risk factors, and institutions should consider implementing mandatory pre-dispensing counseling protocols. The consequences of oversight are not merely theoretical - they are fatal, and entirely preventable with diligence.
Phil Davis
January 30, 2026 AT 16:23Wow. So the real danger isn’t the drug. It’s the fact that we expect people to remember 17 different things they can’t do while wearing a patch that looks like a Band-Aid.
Next they’ll tell me not to sneeze near it. Or blink too hard. Or exist during daylight.
At this point, I’m just waiting for the lawsuit where someone overdoses because their dog licked the patch after they threw it in the trash and the dog got warm from running around the yard. We’ve officially entered the dystopia.
Irebami Soyinka
January 30, 2026 AT 18:32USA still treating pain like a luxury? 😒
Here in Nigeria, we don’t have patches - we have painkillers you swallow and pray you don’t vomit. But at least you know when you’re high. No sneaky heat traps killing folks like they’re in some sci-fi horror movie.
Y’all give people a patch that’s basically a time bomb and then act shocked when it goes off? 🤦♀️
Stop making medicine sound like a video game boss fight. Just give them the right dose. Or don’t give it at all. But don’t pretend this is ‘safe’ if you’re gonna let them take a hot shower and die.
Respect the drug. Respect the patient. Or stop selling death in a sticky square.
🔥💀 #NaijaWise
Kevin Kennett
January 31, 2026 AT 14:00I’ve been on these patches for five years. I never knew heat was a thing until my cousin’s dad died last year. He didn’t do anything wrong. Just had the flu. Got a little fever. Took a warm shower. And that was it.
People think you’re being dramatic if you say you’re scared to sweat. But I don’t turn the AC off. I don’t wear hoodies. I don’t even sit in the car if it’s been sitting in the sun. I check my temperature every morning like it’s my job.
And yeah - I’m tired of being the weird one who won’t go to the spa with the family. But I’m alive. And I’d rather be the weird one than the ghost in the obituary.
If you’re on this patch - please, please, please. Don’t assume it’s fine. It’s not. Heat doesn’t care if you’re ‘just a little warm.’ It doesn’t wait for permission.
Jess Bevis
January 31, 2026 AT 22:41Heat = faster absorption. Simple.
Don’t get hot. Done.
Rose Palmer
February 1, 2026 AT 10:51It is of paramount importance to underscore that the administration of transdermal fentanyl necessitates a comprehensive risk mitigation strategy, inclusive of patient education, environmental control, and vigilant monitoring for signs of respiratory depression. The pharmacological properties of fentanyl, particularly its sensitivity to thermally induced alterations in dermal perfusion, demand a level of patient compliance that is often underestimated in clinical practice.
Healthcare institutions must prioritize structured, multilingual, and visually reinforced patient education protocols to ensure comprehension across diverse populations. Furthermore, the inclusion of a mandatory safety checklist, signed by both provider and patient, should be considered standard of care. Lives depend on this discipline.
Kathy Scaman
February 1, 2026 AT 16:25My mom’s on these. She’s 72. Last week she took a hot bath after her PT session and I freaked out. She was like, ‘It’s just warm water, honey.’
I had to sit her down and read her the whole article. She cried. Said she didn’t know. No one told her.
Now I check her temp every day. We keep the house at 68. She wears socks to bed. I even bought her a little thermometer that beeps if it’s over 99.5.
It’s exhausting. But I’d rather be annoying than bury her.
Also - don’t even get me started on the damn patch disposal. I fold it like it’s a bomb. I hide it like it’s a secret. I’m not taking chances.
Rhiannon Bosse
February 2, 2026 AT 21:59Okay but what if this is all a big pharma scam to sell more naloxone? 🤔
Think about it. They make a patch that’s basically a slow-motion opioid grenade, then they charge you $500 for it, then they tell you not to breathe near it, then they sell you $100 naloxone kits like it’s a survival pack for your living room.
And the worst part? They know most people won’t read the warning. So they bury it in 12-point font under ‘Important Safety Information’ like it’s a hidden level in a game.
And then they act shocked when someone dies. ‘Oh no! We warned them!’
Yeah, you warned them in a 300-page booklet that came with a sticker that says ‘DO NOT USE WITH HEAT’ in letters smaller than a mosquito’s eyelash.
Y’all aren’t saving lives. You’re monetizing fear.
And don’t even get me started on the ‘folding the patch’ thing. I swear someone’s gonna die because they tried to peel it off and it stuck to their kid’s finger. Then the kid goes to school and hugs someone. And now the whole class is high.
WHO DESIGNED THIS SYSTEM?! 😭
Lance Long
February 3, 2026 AT 18:17I’ve been on fentanyl patches for 8 years. I’ve had pneumonia, the flu, a fever of 102. I’ve sat in a sauna, I’ve taken hot showers, I’ve worn three layers in July. And I’m still here.
Let me tell you something - your body adapts. You learn. You feel the difference. That dizzy, foggy, ‘I’m melting’ feeling? That’s your body screaming. I stop. I cool down. I call my doctor.
Yes, heat is dangerous. But so is panic. So is fear. So is letting a piece of paper scare you into thinking you can’t live.
I don’t live in a bubble. I live with this. And I’m not dying because someone didn’t explain it well enough. I’m living because I paid attention.
To everyone else - listen. Learn. Don’t be reckless. But don’t let fear steal your life either.
There’s a middle ground. And it’s called awareness. Not paranoia.
And yes - I still take hot showers. But I keep the timer on. And I don’t let it go past 7 minutes.
It’s not about never getting warm. It’s about knowing when to cool down.
And if you don’t know? Call your doctor. Don’t Google it. Don’t read Reddit. Call them. They’re paid to help you. Use them.
Jeffrey Carroll
February 4, 2026 AT 10:41While the anecdotal experiences shared by other commenters are compelling, it is essential to distinguish between individual tolerance and population-level risk. The pharmacokinetic variability among patients - particularly the elderly, those with hepatic impairment, or those on CYP3A4 inhibitors - renders generalized assumptions about safety untenable.
One individual’s resilience does not negate the documented mortality rate associated with thermal exposure. The responsibility of the medical community is not to validate personal exceptions, but to prevent predictable tragedies through systemic safeguards.
Education must be standardized, not optional. And warnings must be unambiguous, not buried.