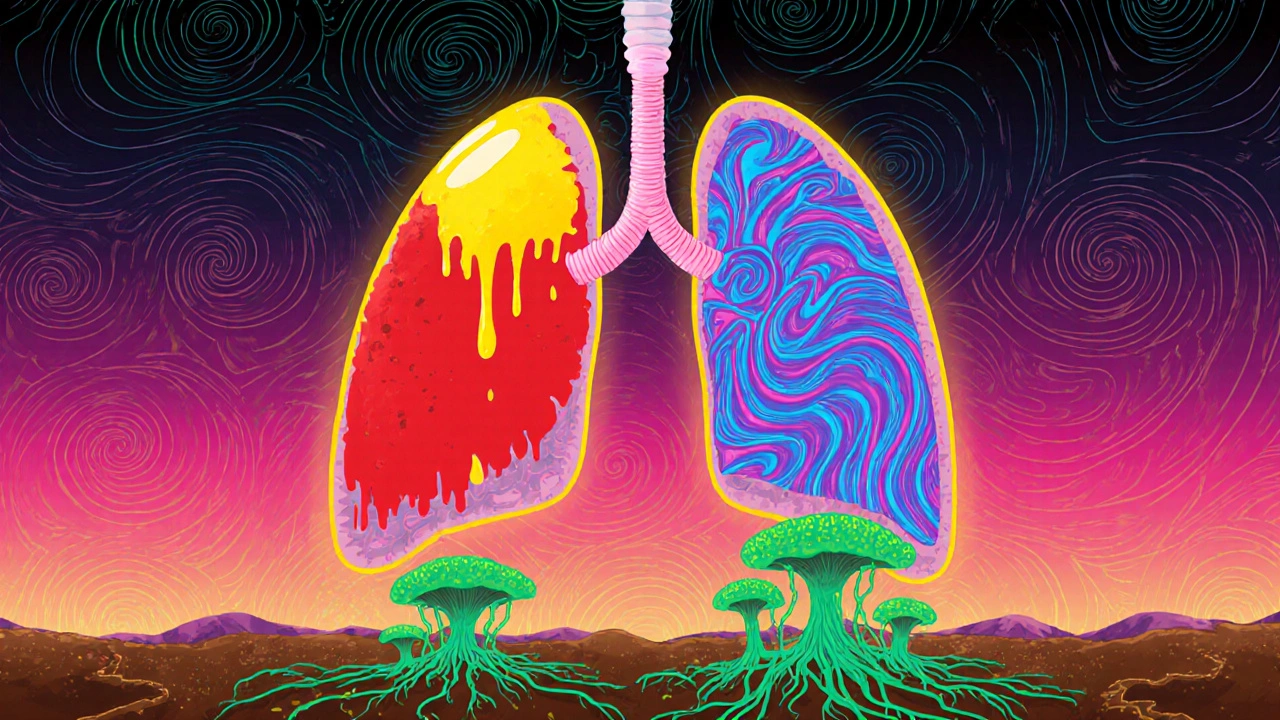
When fungal pneumonia, a lung infection caused by fungi that enter the respiratory system and trigger inflammation. Also known as invasive fungal pneumonia, it’s not something you catch from a coworker or a cold day—it’s a serious threat mostly to people with weakened immune systems. Unlike bacterial or viral pneumonia, fungal pneumonia doesn’t spread person to person. It comes from breathing in spores from soil, bird droppings, or decaying organic matter—things like histoplasma, coccidioides, or aspergillus. These fungi are everywhere, but for most people, the immune system handles them without a second thought. For others—those on chemotherapy, after organ transplants, living with HIV, or taking long-term steroids—it’s a different story.
That’s why antifungal medications, drugs designed to kill or slow the growth of fungi in the body are critical. Medications like voriconazole, amphotericin B, and fluconazole aren’t just prescriptions—they’re lifelines. But they’re not simple. They can strain your kidneys, interact with other drugs like immunosuppressants, and need careful dosing based on weight, liver function, and how far the infection has spread. Many patients don’t realize that treating fungal pneumonia isn’t a quick fix. It often takes weeks or months, and sometimes surgery is needed if the infection forms a mass in the lung.
The people most at risk are often managing other chronic conditions. That’s why immunocompromised, a state where the body’s ability to fight off infections is reduced is such a key term here. If you’re on azathioprine or mycophenolate after a transplant, or taking high-dose steroids for autoimmune disease, you’re already on a tightrope. Adding fungal pneumonia into the mix means you need more than just antifungals—you need a full care plan. That includes tracking every medication you take, avoiding places with heavy dust or mold, and knowing the early signs: persistent cough, fever that won’t break, shortness of breath that gets worse over days, not hours.
And here’s the thing most doctors don’t stress enough: fungal pneumonia is often misdiagnosed. It looks like bacterial pneumonia on a chest X-ray. If you’ve been on antibiotics for a week and still feel awful, ask about fungal testing. A simple blood test or sputum culture can change everything. Delayed diagnosis means worse outcomes.
Below, you’ll find real, practical advice from people who’ve been there. You’ll see how to keep a medication list that keeps you safe, how to time your pills to avoid dangerous interactions, and what to ask your doctor when you’re told a generic version will work just fine. You’ll learn how to spot the warning signs before it’s too late—and how to talk to your care team when you know something’s off. This isn’t theory. It’s what works when your lungs are fighting more than just a cold.
Learn the key differences between bacterial, viral, and fungal pneumonia-how they start, how they’re treated, and who’s most at risk. Get clear, science-backed info to understand your symptoms and when to seek help.