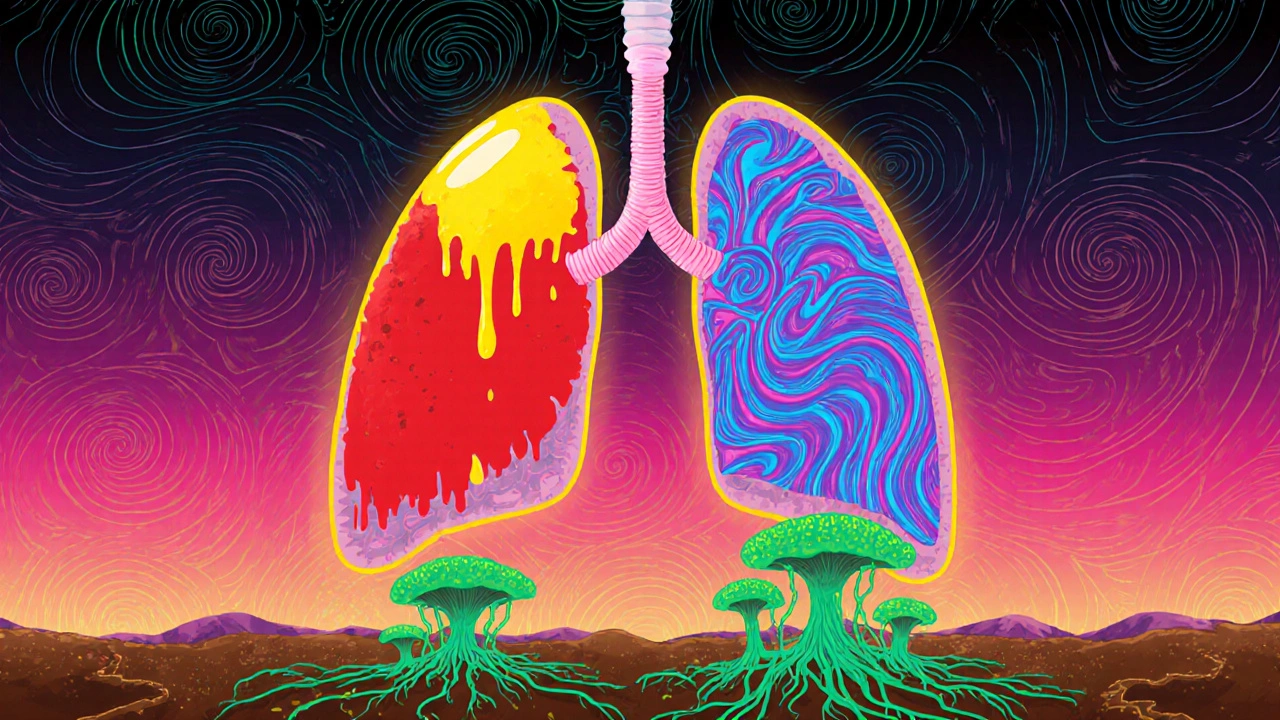
When your lungs start to feel heavy, your chest aches, and breathing becomes a chore, it’s easy to assume it’s just a bad cold. But if symptoms don’t improve after a few days-or get worse-you could be dealing with pneumonia. Unlike a simple cold, pneumonia is an infection that fills the tiny air sacs in your lungs with fluid or pus, making it hard to get enough oxygen into your bloodstream. Not all pneumonia is the same. The cause changes everything: how it starts, how it feels, how it’s treated, and how dangerous it can be.
Bacterial Pneumonia: The Sudden Onset
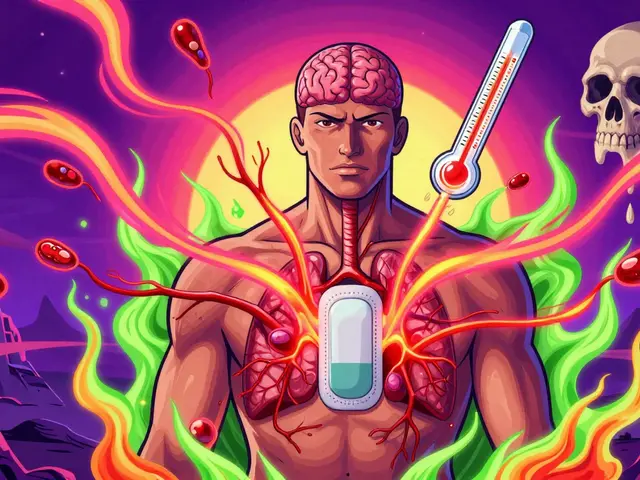
Bacterial pneumonia is the most common type, responsible for about half of all community-acquired cases. The main culprit? Streptococcus pneumoniae. This bacteria doesn’t just show up out of nowhere-it often follows a cold or flu, especially in people with weakened defenses. It’s the leading cause of pneumonia in children under five and adults over 65. The symptoms hit fast. One day you might feel fine; the next, you’re running a fever of 103°F to 105°F, shivering, and coughing up thick, yellow or green mucus. You might feel sharp pain when you breathe or cough, and your lips or fingernails could turn blue because your body isn’t getting enough oxygen. Your heart races, your breathing is shallow, and you feel exhausted even when you’re not moving. On a chest X-ray, bacterial pneumonia usually shows up as one solid white patch in a single lobe of the lung-a sign of lobar consolidation. That’s because the infection is localized, not scattered. Doctors often hear crackling sounds or reduced breath sounds when listening with a stethoscope on the affected side. Treatment is straightforward if caught early: antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin work well against common strains. But here’s the catch: if you take antibiotics when you don’t need them, you’re helping bacteria become stronger. The CDC estimates that 30% of antibiotic prescriptions in outpatient settings are unnecessary, mostly because viral infections are mistaken for bacterial ones.Viral Pneumonia: The Slow Burn
Viral pneumonia makes up about one-third of all cases. It’s caused by the same viruses that give you the flu or a bad cold-influenza A and B, RSV, rhinovirus, and SARS-CoV-2 (the virus behind COVID-19). Unlike bacterial pneumonia, it doesn’t usually come on with a bang. It creeps in. You might start with a runny nose, sore throat, and mild fever. After a few days, you feel worse: dry cough, muscle aches, fatigue, and a low-grade fever around 100°F to 102°F. The cough gets worse over time, but you rarely cough up thick mucus. Breathing feels tight, and you might feel short of breath even when sitting still. On an X-ray, viral pneumonia looks different. Instead of one solid white patch, you’ll see a hazy, widespread pattern across both lungs. That’s because the virus attacks the tissue between the air sacs, not the sacs themselves. It triggers a broader inflammatory response, flooding the lungs with fluid and immune cells. Antibiotics won’t help here. Treatment is mostly rest, fluids, and fever reducers. In some cases-especially with severe flu or COVID-19-doctors may prescribe antivirals like oseltamivir or remdesivir. But timing matters. These drugs work best if started within 48 hours of symptoms. One of the biggest dangers with viral pneumonia is what comes next: bacterial superinfection. About 25% to 30% of people with severe flu or COVID-19 pneumonia develop a secondary bacterial infection, usually from Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely-if someone with viral pneumonia suddenly spikes a high fever or starts coughing up pus, they may need antibiotics.Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. You won’t catch it from someone else. Instead, you breathe in spores from the environment-soil, bird droppings, decaying wood. It’s most dangerous for people with weak immune systems: those with HIV, cancer patients on chemo, organ transplant recipients, or anyone on long-term steroids. The three main fungi that cause pneumonia in the U.S. are Coccidioides (Valley fever), Histoplasma, and Blastomyces. They’re not rare in certain regions. Coccidioides is common in the Southwest, especially Arizona and California. Histoplasma hides in the soil of the Ohio and Mississippi River valleys. Blastomyces shows up in damp, wooded areas of the Midwest and Southeast. Symptoms are sneaky. Fever, cough, chills, fatigue-sound familiar? They mimic bacterial or viral pneumonia. But fungal pneumonia can also cause joint pain, night sweats, or even skin rashes. Some people don’t feel sick at all. Others develop chronic lung problems that last months. Diagnosing it is hard. Standard tests often miss it. Doctors need special tests: sputum cultures, blood tests for fungal antigens, or biopsies. Chest X-rays might show nodules or cavities, not the clear lobar patch seen in bacterial cases. Treatment isn’t antibiotics. It’s antifungals-drugs like fluconazole, itraconazole, or stronger ones like amphotericin B for severe cases. Treatment can last for months, sometimes years. Without it, fungal pneumonia can spread beyond the lungs to the brain, skin, or bones.
Who’s at Risk?
Anyone can get pneumonia, but some groups are far more vulnerable:- Children under 2 and adults over 65
- People with chronic lung disease (COPD, asthma)
- Those with heart disease, diabetes, or kidney disease
- Smokers (they’re 2.3 times more likely to get pneumonia)
- People with weakened immune systems
- Workers exposed to dust and spores: farmers, landscapers, construction crews
How to Tell Them Apart
It’s not always easy to know which type you have just from symptoms. But here’s a quick guide:| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden, severe | Gradual, over days | Slow, sometimes weeks |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Moderate to high |
| Cough | Productive, thick mucus | Dry or minimal mucus | Productive, sometimes with blood |
| Chest X-ray | One lobe, solid white patch | Bilateral, hazy, scattered | Nodules, cavities, or diffuse infiltrates |
| Key Risk Factors | Age, smoking, recent illness | Flu season, crowded spaces | Soil exposure, immunosuppression |
| Treatment | Antibiotics | Rest, antivirals (if early) | Antifungals (long-term) |

Prevention: What Actually Works
You can’t always avoid germs, but you can reduce your risk:- Pneumococcal vaccines (PCV20 or PPSV23) cut bacterial pneumonia risk by 60-70% in kids and 45-75% in adults. Despite this, only 68% of adults over 65 are vaccinated.
- Flu shots reduce pneumonia risk by 40-60% during flu season. They’re especially critical for older adults.
- COVID-19 vaccines lower pneumonia risk by up to 90% in the months after vaccination.
- Quit smoking. Your lungs heal over time. Even after years of smoking, quitting cuts pneumonia risk by half within a decade.
- Wear a mask in high-risk environments-construction sites, farms, or during flu season in crowded places.
- Wash your hands. Simple, but it blocks the spread of viruses and bacteria.
What’s Next in Diagnosis and Treatment
New tools are making it easier to know what you’re dealing with. Multiplex PCR tests can now check a single nasal swab for over 20 different viruses and bacteria in under 24 hours-with 95% accuracy. That means doctors can stop guessing and start treating faster. Researchers are also working on blood tests that detect your body’s immune response. If your body is fighting a virus, it releases different signals than if it’s fighting bacteria. These biomarkers could soon tell doctors whether antibiotics are needed-even before test results come back. New pneumococcal vaccines like Prevnar 20 protect against 20 strains instead of 13, offering broader coverage. They’re already approved for adults and are being rolled out to children.When to Seek Help
Don’t wait to see if it gets better. Call a doctor if you have:- Fever above 102°F that doesn’t go down
- Coughing up blood or thick green/yellow mucus
- Shortness of breath that gets worse
- Chest pain when breathing
- Lips or nails turning blue
- Confusion or dizziness (especially in older adults)
Can you get pneumonia from the flu?
Yes. Viral pneumonia can be caused directly by the flu virus. But even more common is a secondary bacterial infection that follows the flu. About 25-30% of severe flu cases lead to bacterial pneumonia, often from Streptococcus pneumoniae. That’s why flu vaccines are one of the best ways to prevent pneumonia.
Is fungal pneumonia contagious?
No. Fungal pneumonia isn’t spread from person to person. You get it by breathing in spores from the environment-soil, bird droppings, or decaying wood. People with healthy immune systems usually don’t get sick from it. But those with weakened immunity can develop serious lung infections.
Do antibiotics work for viral pneumonia?
No. Antibiotics only kill bacteria. They have no effect on viruses. Taking them for viral pneumonia doesn’t help you get better faster. Instead, it increases the risk of antibiotic-resistant infections, which are harder to treat. Only use antibiotics if a doctor confirms a bacterial infection.
How long does pneumonia last?
It depends on the type and your health. Bacterial pneumonia often improves in 3-5 days with antibiotics, but full recovery can take 2-4 weeks. Viral pneumonia may last 1-3 weeks, with fatigue lingering longer. Fungal pneumonia can take months to treat and sometimes requires lifelong medication in people with weak immune systems.
Can pneumonia come back after treatment?
Yes. If you don’t finish your antibiotics, the infection can return. People with chronic lung disease, smokers, or those with weakened immunity are more likely to get pneumonia again. Getting vaccinated and avoiding triggers like smoke or dust helps prevent recurrence.





Rachael Gallagher
November 25, 2025 AT 12:40They say antibiotics save lives but honestly? Most docs just prescribe them like candy. I’ve seen people take them for colds and then get worse. It’s not medicine-it’s laziness with a prescription pad.
steven patiño palacio
November 27, 2025 AT 08:30Great breakdown. The distinction between bacterial and viral pneumonia is critical-not just for treatment but for public health. Antibiotic stewardship isn’t optional anymore; it’s survival. Thanks for clarifying the X-ray patterns too; that’s something even med students overlook.
stephanie Hill
November 27, 2025 AT 12:53Did you know the government’s been hiding the truth about fungal pneumonia? They don’t want you to know how much mold is in your air conditioning, your office building, your damn water supply. It’s not just soil-it’s engineered. They’ve been spraying spores since the 90s to keep us docile. Look at the stats-cases spike right after new buildings open. Coincidence? I think not.
Jacob McConaghy
November 27, 2025 AT 13:28My uncle had fungal pneumonia after his transplant. Took him two years to recover. They put him on fluconazole and he still gets checked every six months. It’s wild how something you breathe in from dirt can turn into a lifelong battle. People don’t get it unless it hits their family.
Jeff Hicken
November 29, 2025 AT 07:58so like... wait u mean antibiotics dont work on viruses??? wow. mind blown. i thought all germs were the same lol. also why is everyone so scared of pneumonia? i got a cough last year and drank hot tea and it went away. maybe we just need to chill??
Adam Hainsfurther
November 30, 2025 AT 11:21The multiplex PCR tests mentioned are a game-changer. I work in a rural clinic-we used to wait days for cultures. Now we get results in hours. That means we can stop guessing and start treating. It’s not perfect, but it’s the closest we’ve come to precision medicine for pneumonia in primary care.
Akash Chopda
December 1, 2025 AT 12:42Nikki C
December 1, 2025 AT 22:17It’s funny how we treat lungs like they’re just pipes. They’re not. They’re alive. They remember. Smoke, pollution, even stress-they all leave marks. And when pneumonia hits, it’s not just an infection. It’s the body screaming that it’s been pushed too far for too long. We fix the symptom, not the story.