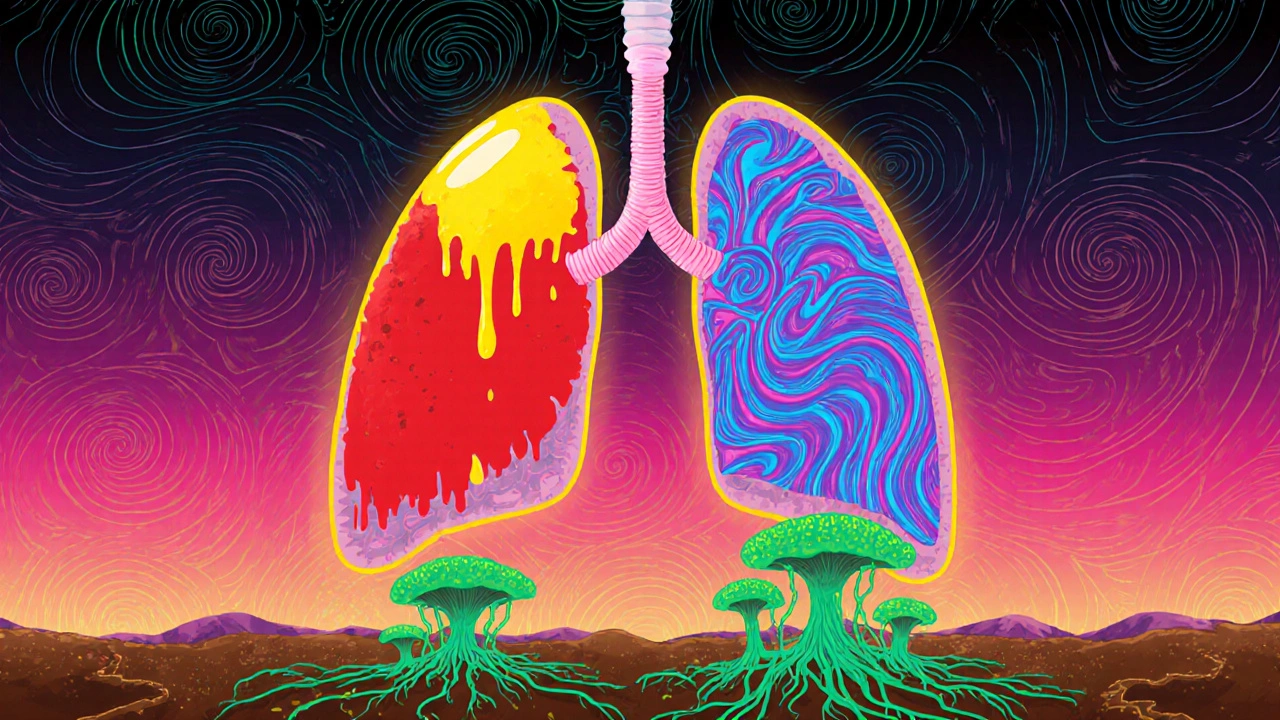
When bacterial pneumonia, a lung infection caused by bacteria like Streptococcus pneumoniae that fills the air sacs with fluid or pus. Also known as community-acquired pneumonia, it's one of the most common reasons people end up in the hospital—especially after a cold or flu weakens their defenses. Unlike viral pneumonia, which often clears on its own, bacterial pneumonia usually needs antibiotics to stop the infection from spreading. If you're coughing up thick mucus, have a high fever, or feel like you can't catch your breath, it’s not just a bad cold—it could be this.
What makes bacterial pneumonia tricky is that it doesn’t always look the same. Some people get sick fast, with chills and sharp chest pain. Others, especially older adults or those with weak immune systems, might just feel tired, confused, or lose their appetite. That’s why doctors often check oxygen levels, listen to your lungs, and sometimes order a chest X-ray. Treatment usually starts with antibiotics, medications that kill or slow the growth of bacteria causing the infection like amoxicillin, azithromycin, or doxycycline. But timing matters. Taking them too late, skipping doses, or stopping early because you feel better can lead to resistance or a return of the infection.
And here’s something most people don’t think about: antibiotic side effects, unwanted reactions like diarrhea, nausea, or yeast infections that often come with antibiotic use can make recovery harder. If you’re already dealing with stomach issues from the infection, adding a probiotic at the right time can help. Studies show taking probiotics 2 hours after your antibiotic dose reduces the chance of antibiotic-associated diarrhea by up to 42%. That’s not just a nice-to-have—it’s part of smart treatment.
People with chronic lung conditions like COPD or asthma are at higher risk, and that’s why managing those diseases matters just as much as treating the pneumonia itself. If you’ve had pneumonia before, keeping a clear list of your meds—especially inhalers or steroids—can help your doctor avoid dangerous interactions. Some antibiotics can mess with blood thinners, seizure meds, or even your heart rhythm. It’s not just about killing the infection; it’s about protecting your whole system.
Recovery doesn’t end when the fever breaks. You might feel weak for weeks. That’s normal. But if you’re still coughing after 3 weeks, or your breathing gets worse again, you might need another look. Sometimes the infection clears but leaves behind inflammation that needs different treatment. And if you’re over 65, diabetic, or on immunosuppressants, your doctor might recommend vaccines like pneumococcal PCV20 to lower your risk next time.
Below, you’ll find real guides from people who’ve walked this path—how to track your meds safely, what to do if antibiotics don’t work, how to avoid side effects, and why some people need longer treatment than others. No fluff. Just what actually helps when you’re fighting a lung infection.
Learn the key differences between bacterial, viral, and fungal pneumonia-how they start, how they’re treated, and who’s most at risk. Get clear, science-backed info to understand your symptoms and when to seek help.