Switching from a brand-name medication to a generic might sound like a simple cost-saving move-but for some people, it’s not. If you’ve noticed changes in how you feel after your pharmacy filled a generic version of your prescription, you’re not alone. In fact, many patients report differences in effectiveness, side effects, or even how the pill tastes or smells. And while generics are required by law to be bioequivalent to their brand-name counterparts, the reality for some is more complicated. If you need to stay on your brand medication, knowing how to talk to your doctor about it can make all the difference.
Why Some People Can’t Switch to Generics
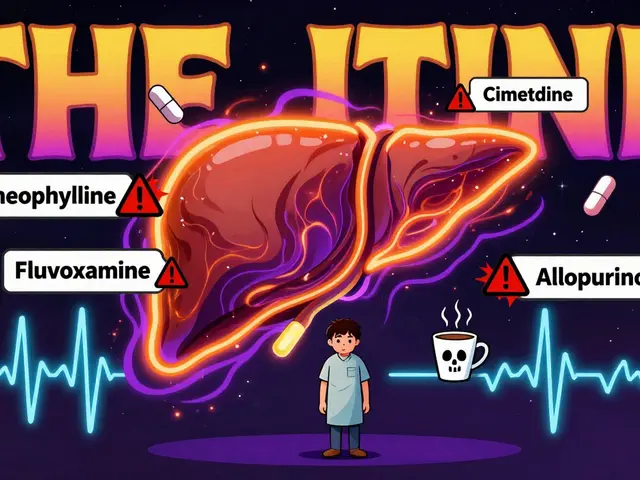
Not all medications are created equal when it comes to switching. For drugs with a narrow therapeutic index-like levothyroxine for thyroid conditions, warfarin for blood thinning, or certain anti-seizure medications-small changes in how the drug is absorbed can lead to big problems. Studies show that switching from brand-name Keppra to a generic version led to a 23% increase in seizure recurrence in some patients. With warfarin, patients who switched between different generic brands had a 17% higher chance of ending up in the emergency room due to unstable blood levels. It’s not just about the active ingredient. Generics can have different fillers, dyes, or preservatives. If you’re allergic to lactose, gluten, or certain food dyes like FD&C Yellow No. 5, you might react to a generic version-even if the active drug is the same. About 7% of patients report adverse reactions to these inactive ingredients, according to the Journal of Allergy and Clinical Immunology. Some people don’t have allergies but still feel off. They might describe it as “the generic doesn’t work like the brand did.” That’s not just in their head. Pharmacists report that 63% of them have seen cases where patients clearly responded differently to generics, especially with psychiatric or neurological drugs.What to Do Before Your Appointment
Don’t walk into your doctor’s office saying, “I just don’t like the generic.” That won’t cut it. You need evidence. Start by keeping a simple journal. Write down:- The date you switched to the generic
- What symptoms changed (fatigue, headaches, mood swings, seizures, etc.)
- How severe they were (on a scale of 1-10)
- When they improved after going back to the brand
How to Talk to Your Doctor
Doctors are busy. They’re also under pressure from insurers to prescribe generics. So you need to be clear, calm, and specific. Use the SBAR method:- Situation: “I’ve been on Brand X for five years. Last month, I switched to the generic, and within a week, I started having severe headaches and feeling dizzy.”
- Background: “I’ve never had these symptoms before. I’ve kept a log of my symptoms and my last INR reading dropped from 2.8 to 1.9 after the switch.”
- Assessment: “I believe this change is linked to the generic. When I went back to the brand, my symptoms disappeared and my INR stabilized.”
- Recommendation: “Can we keep me on the brand? I’m happy to sign a form or provide my lab results.”
Insurance and the Paperwork Hurdle
Even if your doctor agrees, your insurance might not. Most commercial plans require prior authorization for brand-name drugs when a generic is available. That means your doctor has to fill out forms explaining why the brand is medically necessary. You can help by giving your doctor:- Your symptom journal
- Lab results showing instability
- Documentation of allergic reactions to inactive ingredients
- A copy of the FDA’s Orange Book entry for your drug
What If Your Doctor Says No?
Sometimes, doctors push back because they’re pressured by insurers or they believe generics are always fine. If that happens, ask:- “Can you refer me to a specialist who’s more familiar with this drug’s behavior in patients?”
- “Can we try a different generic manufacturer? Some brands of the same generic work better than others.”
- “Is there a biosimilar or another brand alternative I could try?”
What’s Changing in 2025
The FDA has started cracking down on generic drug quality. In 2023, 22% of foreign manufacturing facilities received complete response letters-up from 15% in 2022. That means more scrutiny on the quality of generics. The CREATES Act, now in full effect, prevents brand-name companies from blocking generic access. And in January 2024, Medicare started penalizing brand-name drug makers for price hikes above inflation. That could mean less pressure to switch patients to generics in the future. Long-term, pharmacogenomics-testing your genes to see how you metabolize drugs-might make this whole debate easier. Soon, doctors may know exactly which formulation works best for you based on your DNA. For now, though, your experience matters. If you’ve tried the generic and it didn’t work, you have the right to speak up.Can I just ask my pharmacist not to substitute my brand medication?
In most states, pharmacists can switch your brand medication to a generic without telling you-unless your doctor writes “Dispense as Written” (DAW-1) on the prescription. You can ask your pharmacist to hold the brand version, but they’re legally allowed to substitute unless the prescription specifically says otherwise. The only way to guarantee you get the brand is to have your doctor write DAW-1 and provide medical justification.
Are generics really as good as brand-name drugs?
For most medications, yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also be absorbed into the bloodstream at the same rate and extent. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or seizure meds-small differences in absorption can matter. About 14% of doctors report seeing different effects in patients after switching. That’s why personal experience matters.
What if I can’t afford the brand medication?
You’re not alone. Many brand-name drugs cost hundreds more than generics. Ask your doctor about patient assistance programs offered by the manufacturer. Many drug companies have free or low-cost programs for people with low income. You can also check with nonprofit organizations like NeedyMeds or the Patient Advocate Foundation. Some pharmacies offer discount cards that lower the price of brand-name drugs. Don’t skip your medication because of cost-there are options.
Can I switch back to the brand if the generic isn’t working?
Yes, and you should. If you notice new or worsening symptoms after switching, go back to the brand as soon as possible. Keep track of when the symptoms started and when they improved. This timeline is your strongest evidence when talking to your doctor. Don’t wait until you’re in crisis-acting early gives you better data to support your case.
Do I need to tell my doctor every time I refill my prescription?
No, not if your doctor has written DAW-1 on the prescription and your insurance has approved it. Once the exception is in place, your pharmacy should automatically fill the brand version. But if you notice a generic was dispensed anyway, contact your doctor’s office immediately. Sometimes, pharmacies make mistakes or switch suppliers without notice. Keep your prescription label and call your doctor if something looks off.





Bill Camp
November 20, 2025 AT 15:10This is why America’s healthcare system is broken. Big Pharma bribes doctors, insurers screw patients, and the FDA lets generic manufacturers cut corners while pretending it’s all the same. I’ve seen people go from stable to seizures because some Chinese factory decided to use cheaper lactose filler. We need to ban these knockoffs entirely. If your life depends on it, you deserve the real thing - not some lab’s leftover batch.
Lemmy Coco
November 21, 2025 AT 00:07just wanted to say i switched from brand keppra to generic and my seizures got worse by like 40%... i didnt even realize it at first because the headaches started slow. kept a journal like the article said and brought it to my neuro. they finally agreed to daw-1 after seeing my logs. took 3 months but worth it. also found out my generic had red 40 and i’m allergic. who knew?
rob lafata
November 22, 2025 AT 15:09Oh here we go. The ‘I feel different’ crowd. Let me guess - you didn’t even check your blood levels? You think your ‘gut feeling’ overrides clinical data? You’re not special. Your brain is just hypersensitive because you’re anxious. The FDA doesn’t approve generics based on vibes. If your INR fluctuated, that’s poor management - not the drug. Stop blaming generics and start taking responsibility for your own health. Also, you’re probably just paranoid because you read too many Reddit threads.
Matthew McCraney
November 24, 2025 AT 06:50They’re poisoning us. Did you know the FDA gets money from Big Pharma to approve these generics? The same companies that make the brand names own the generic factories. That’s why they say they’re ‘bioequivalent’ - it’s a lie. I switched to generic levothyroxine and my thyroid went haywire. Then I found out the capsule had titanium dioxide - a known neurotoxin. They’re testing us. This is how they control the population. I’ve been tracking every pill I take since 2021. I’m not taking another generic. Ever.
Nick Naylor
November 24, 2025 AT 10:48Let’s be clear: The FDA’s AB rating system is a flawed, outdated metric. For drugs with a narrow therapeutic index - such as warfarin, levothyroxine, phenytoin, carbamazepine, cyclosporine, and tacrolimus - the 80-125% bioequivalence window is not sufficient for clinical safety. Variability in dissolution profiles, excipient interactions, and gastric pH dependency can cause clinically significant deviations. Therefore, the presumption of interchangeability is medically indefensible. DAW-1 is not a request - it is a clinical imperative. And if your insurer denies it? Appeal. Document. Escalate. Repeat. This isn’t opinion - it’s pharmacokinetics.
Brianna Groleau
November 24, 2025 AT 13:55I’m a nurse, and I’ve seen this over and over. Patients come in crying because they feel ‘off’ after switching - exhausted, anxious, foggy, or worse. And the first thing the doctor says is, ‘It’s all in your head.’ But when we look at their logs, their lab results, their symptom timelines - it’s not in their head. It’s in the pill. I had a patient on brand Lamictal who started having panic attacks after switching. She was a teacher, couldn’t get through a class. Went back to brand - vanished. No new diagnoses, no new stressors. Just a different filler. We need to stop treating people like numbers. Your body knows when something’s wrong. Trust it. And if your doctor won’t listen? Find one who will.
Rusty Thomas
November 26, 2025 AT 13:22OMG YES. I switched to generic warfarin and almost died. My INR dropped to 1.2. I was dizzy for weeks. I thought I was having a stroke. Then I went back to brand - boom, back to 2.5. I cried in the pharmacy. The pharmacist just shrugged and said, ‘It happens.’ Well, it shouldn’t. I’ve been on this drug for 12 years. I know my body. And now I keep the brand pill in a little box on my nightstand with a note: ‘DO NOT SUBSTITUTE.’ I’ve even printed out the FDA Orange Book page and taped it to my prescription bottle. If you’re reading this and you’re on a generic that’s not working? You’re not crazy. You’re just not being heard.
Sarah Swiatek
November 28, 2025 AT 04:22It’s funny how we treat medicine like it’s a soda - ‘same taste, cheaper price.’ But your body isn’t a vending machine. It doesn’t just ‘absorb the active ingredient’ and call it a day. It’s a living, breathing ecosystem that reacts to every micro-particle in that pill - the dye, the binder, the coating, the humidity the factory stored it in. And yet, we treat patients like they’re just data points. The real tragedy isn’t that generics sometimes fail - it’s that we’ve normalized ignoring people’s lived experience. You don’t need a PhD to know when something’s off. You just need to be listened to. Maybe the real innovation isn’t in the pill - it’s in the way we listen.
Dave Wooldridge
November 28, 2025 AT 21:44They’re putting tracking chips in the generics. I saw it on a documentary. The same company that makes the brand also makes the generic - and they’re using the fillers to monitor your biometrics. That’s why they say it’s ‘bioequivalent’ - because they need you to swallow it so they can track you. I stopped taking all generics. Now I only take brand. I even have my pills shipped from Canada. I don’t trust the FDA. I don’t trust the pharmacy. I don’t trust anyone. But I trust my body - and my body says: NO MORE.