SGLT2 Inhibitor Risk Calculator
Assess Your Risk
Answer these 5 questions to determine your risk level for urinary complications while taking SGLT2 inhibitors.
Results
You have a low risk of complications. Continue with your current medication but maintain good hygiene practices and stay hydrated. Contact your doctor if you notice any unusual symptoms.
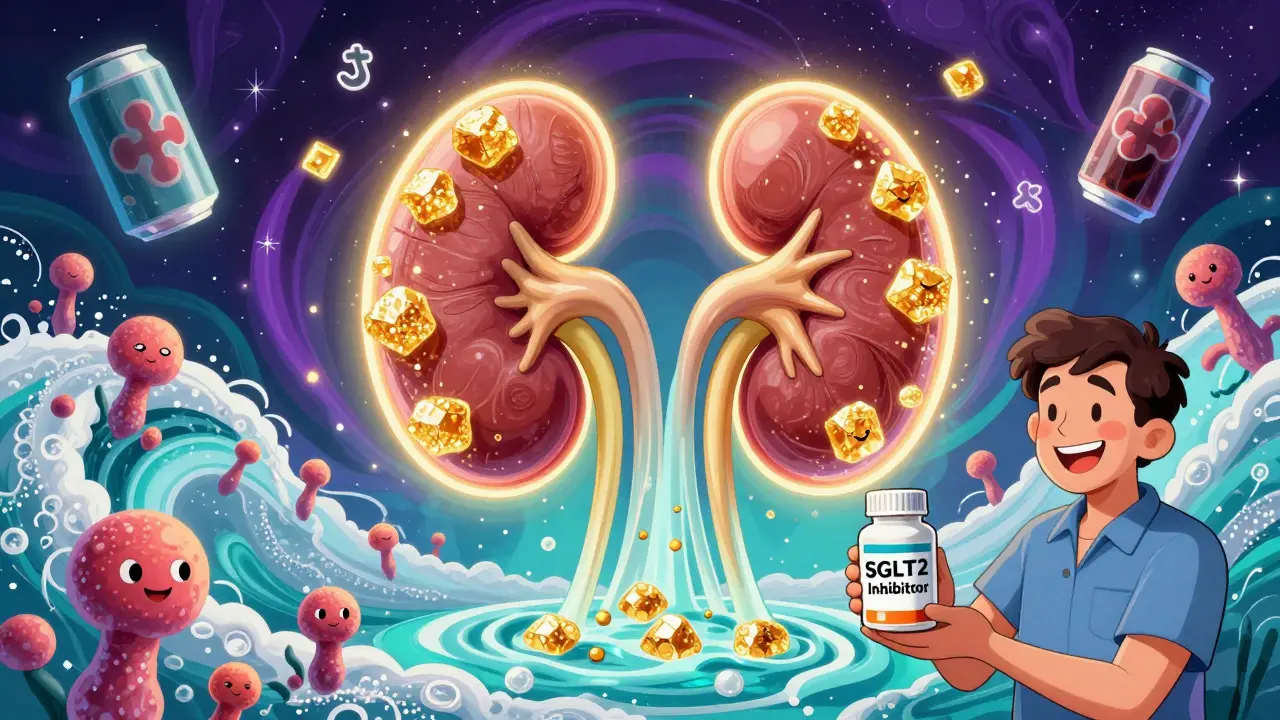
When you're managing type 2 diabetes, finding a medication that lowers blood sugar without causing low blood sugar or weight gain feels like a win. That’s why SGLT2 inhibitors became so popular. Drugs like canagliflozin, dapagliflozin, and empagliflozin work by making your kidneys flush out extra sugar through urine. It sounds simple-and it is. But that same mechanism is also why some people end up with painful yeast infections or serious urinary tract problems.
How SGLT2 Inhibitors Work-and Why They Cause Infections
SGLT2 inhibitors block a protein in your kidneys that normally reabsorbs glucose. Instead of getting pulled back into your bloodstream, sugar gets flushed out in your urine. On average, people taking these drugs lose 40 to 110 grams of glucose per day through urination. That’s like emptying a soda can’s worth of sugar into your bladder every day. This creates a sweet environment for yeast and bacteria. Candida albicans, the fungus that causes most vaginal yeast infections, thrives on sugar. Men and women alike can develop genital itching, redness, or discharge within weeks of starting the medication. In women, vulvovaginal candidiasis is the most common issue. In men, it’s balanitis-an inflammation of the head of the penis. Studies show about 3% to 5% of people on SGLT2 inhibitors get these infections, compared to just 1% to 2% on placebo. But it’s not just about itching. The sugar in your urine doesn’t just attract yeast-it can also feed bacteria like E. coli, leading to urinary tract infections (UTIs). These aren’t always mild. A 2022 meta-analysis found that SGLT2 inhibitors increase the risk of UTIs by nearly 80% compared to other diabetes drugs like DPP-4 inhibitors or sulfonylureas. For some, it’s a one-time annoyance. For others, it’s a recurring problem that leads to hospitalization.The Real Danger: When a UTI Turns Deadly
Most yeast infections are treatable with over-the-counter antifungals. But UTIs on SGLT2 inhibitors can turn dangerous fast. The U.S. Food and Drug Administration (FDA) reviewed reports from 2013 to 2014 and found 19 cases of urosepsis-when a UTI spreads to the bloodstream-linked to these drugs. Ten of those cases involved canagliflozin, nine involved dapagliflozin. All 19 patients needed hospital care. Four ended up in intensive care. Two needed dialysis because their kidneys failed. One case from the National Institutes of Health tells the whole story. A 64-year-old woman with no history of urinary problems started taking dapagliflozin. Within six weeks, she developed emphysematous pyelonephritis-a rare, gas-forming kidney infection that can destroy tissue. She spent 14 days on IV antibiotics. Months later, after restarting the drug, she got another kidney infection and a perinephric abscess. She needed surgery. Her words? “I never had urinary problems before this medication. Now I’ve had two life-threatening infections.” Even rarer-but just as terrifying-is Fournier’s gangrene. This is a necrotizing infection that eats away at the skin and tissue around the genitals and anus. It’s aggressive, fast-moving, and deadly if not caught early. The European Medicines Agency added it to SGLT2 inhibitor warnings in 2016. While only about 1 in 10,000 users experience it, the outcome is often amputation or death.Who’s at Highest Risk?
Not everyone on SGLT2 inhibitors gets infections. But certain people are much more likely to.- Women, especially those who’ve had yeast infections before
- People over 65
- Those with a history of recurrent UTIs
- Patients with poor genital hygiene
- People with diabetes complications like nerve damage (neuropathy) that affects bladder emptying
- Those with kidney function below 60 mL/min/1.73m²
- Patients with HbA1c levels above 8.5%
What Doctors Should Do Before Prescribing
The American Diabetes Association says it clearly: check for a history of urinary infections before starting an SGLT2 inhibitor. If you’ve had three or more UTIs in the past year, consider something else. These drugs shine for people with heart failure or existing heart disease. The EMPA-REG and CANVAS trials showed they cut heart attacks, strokes, and hospitalizations for heart failure by up to 14%. That’s huge. But if you’re young, healthy, and just trying to lower your blood sugar, the infection risk might outweigh the benefit. Endocrinologists now recommend SGLT2 inhibitors as second-line therapy after metformin-but only for patients with heart or kidney disease. For others, DPP-4 inhibitors or GLP-1 receptor agonists (like semaglutide) are safer options with far lower infection risks.What You Can Do to Protect Yourself
If you’re already on an SGLT2 inhibitor and want to avoid problems, here’s what works:- Wipe front to back after using the bathroom. This stops bacteria from entering the urethra.
- Drink plenty of water-at least 2 liters a day. It flushes out sugar and bacteria.
- Change out of wet clothes quickly. Sweaty workout gear or swimsuits are breeding grounds.
- Don’t use scented soaps or douches. They irritate skin and disrupt natural balance.
- Check your genitals daily. Redness, swelling, or unusual discharge? Call your doctor immediately.
- Don’t wait for symptoms to get worse. Fever above 100.4°F, chills, back pain, or nausea? Go to urgent care. Don’t wait for your next appointment.

When to Stop the Medication
If you’ve had one yeast infection, you can often keep taking the drug-just treat it and monitor closely. But if you’ve had two or more infections, or any serious UTI, it’s time to talk about switching. A 2021 study from Sweden showed that nearly 24% of people stopped taking SGLT2 inhibitors within two years because of genitourinary side effects. That’s higher than the rate for other diabetes drugs. If your quality of life is suffering, it’s not weakness to switch. It’s smart.The Bigger Picture: Benefits vs. Risks
SGLT2 inhibitors aren’t bad drugs. They’ve saved lives. They reduce heart failure hospitalizations. They slow kidney disease progression. Global sales hit $12.7 billion in 2022 because they work-really well-for the right people. But they’re not for everyone. The infection risk isn’t a side effect you can ignore. It’s built into the mechanism. And unlike high blood pressure or cholesterol meds, you can’t just take a pill and forget about it. You have to pay attention to your body. For patients with heart disease, the benefits far outweigh the risks. For someone with no cardiovascular issues and a history of UTIs? The risks might be too high.What’s Next?
Researchers are working on new versions of these drugs-dual SGLT1/2 inhibitors-that might cause less sugar to spill into the urine. There are also new risk-prediction tools to help doctors pick the right patients. But for now, the message is simple: know your risk. Know the signs. Don’t let embarrassment stop you from speaking up. A yeast infection is embarrassing. A kidney infection that lands you in the ICU? That’s life-changing.Can SGLT2 inhibitors cause yeast infections in men?
Yes. While vulvovaginal yeast infections are more common in women, men can develop balanitis-an inflammation of the head of the penis-due to sugar in the urine promoting fungal growth. Symptoms include redness, itching, swelling, and sometimes a white discharge. It’s treatable with antifungal creams, but if it keeps coming back, talk to your doctor about switching medications.
How long after starting SGLT2 inhibitors do infections usually appear?
Most genital infections occur within the first 3 months of starting the drug. UTIs can show up anytime, but serious cases like urosepsis often appear between 2 and 6 months after beginning treatment. The FDA found the median time to serious infection was 45 days. That’s why early monitoring is critical.
Are there any SGLT2 inhibitors with lower infection risk?
No. All approved SGLT2 inhibitors-canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin-work the same way: they cause sugar to spill into the urine. That’s the mechanism that causes infections. The risk level is similar across all of them. Choosing one over another won’t reduce your chance of yeast or UTI.
Can I take cranberry supplements with SGLT2 inhibitors?
Yes, and many patients find them helpful. A 2023 FDA safety update cited evidence that cranberry products may reduce UTI incidence by 29% in people on these drugs. It’s not a guarantee, but it’s low-risk and may help prevent recurring infections. Talk to your doctor before starting any supplement, especially if you’re on blood thinners or have kidney stones.
Should I stop my SGLT2 inhibitor if I get a yeast infection?
Not necessarily. A single yeast infection doesn’t mean you need to quit. Treat it with antifungals, improve hygiene, and increase fluid intake. But if it happens again-especially within 6 months-talk to your doctor. Recurrent infections are a sign your body isn’t tolerating the drug well, and switching to another class of diabetes medication may be safer.
What are the alternatives to SGLT2 inhibitors if I keep getting infections?
If infections are a problem, DPP-4 inhibitors (like sitagliptin) or GLP-1 receptor agonists (like semaglutide or liraglutide) are safer choices. They lower blood sugar without causing sugar to spill into urine. Metformin is still first-line for most people. If you have heart or kidney disease, your doctor may still recommend an SGLT2 inhibitor-but only after carefully weighing the risks and benefits.





josue robert figueroa salazar
December 25, 2025 AT 16:54david jackson
December 26, 2025 AT 08:28Jody Kennedy
December 27, 2025 AT 22:28christian ebongue
December 28, 2025 AT 05:46jesse chen
December 29, 2025 AT 09:14Joanne Smith
December 29, 2025 AT 17:13Sarah Holmes
December 30, 2025 AT 22:40Jay Ara
December 31, 2025 AT 09:22