Imagine taking three different pills every day just to manage your blood pressure, diabetes, and cholesterol. Now imagine taking just one pill that does it all. That’s the power of combination products-and their generic versions are making this simpler, cheaper, and more effective for millions.
What Are Generic Combination Products?
A combination product is a single medical product that blends two or more types of treatments-like a drug and a device-into one unit. Think insulin pens, drug-eluting stents, or nicotine patches. These aren’t just pills in a bottle. They’re engineered systems: the drug is built into a delivery tool designed for accuracy, ease, and reliability. Generic combination products are the lower-cost versions of these same systems. Once the original brand’s patent expires, manufacturers can copy the drug and device combo, as long as they prove it works the same way. The FDA requires generic versions to match the brand-name product in active ingredients, dose accuracy, and device performance-down to the force needed to activate an auto-injector or the exact rate a patch releases medicine into the skin. This isn’t just about saving money. It’s about fixing a real problem: patients stop taking their meds because it’s too complicated, too expensive, or both.Why Compliance Goes Up With Combination Products
When patients have to manage multiple medications, adherence drops fast. Studies show that moving from one pill a day to two pills a day cuts adherence by about 26%. Add a third, and many just give up. But when you combine those same drugs into one product, adherence jumps by 15-25%. Take insulin pens. Before they existed, people with diabetes had to draw insulin from a vial, load a syringe, and inject it. Mistakes happened often-wrong dose, air bubbles, spills. A Reddit user in the r/Diabetes community said switching to a prefilled pen cut their dosing errors from 3-4 per week to almost zero. That’s not luck. That’s design. Combination products remove steps. No more assembling parts. No more remembering which pill goes with which meal. No more juggling different schedules. One device. One routine. One less thing to forget.The Cost Advantage That Changes Outcomes
Brand-name combination products can cost hundreds of dollars a month. Generic versions? Often 30-80% cheaper. For someone on a fixed income, that’s the difference between taking their medicine and skipping doses. The FDA found that 23.4% of patients skip doses because of cost. That number drops sharply when generics are available. In fact, studies show patients started on generic medications are 8.7 percentage points more likely to stick with their regimen than those started on brand-name versions. This isn’t theoretical. In Australia, where generic substitution is common, patients on generic combination products for hypertension and COPD report higher persistence rates. They’re not just filling prescriptions-they’re taking the medicine consistently.
How Generic Versions Match the Original
Some people worry that generics are “weaker” or “less reliable.” That’s not true for combination products. The FDA requires generic versions to meet the same strict standards as the brand:- Drug bioequivalence: The amount of medicine absorbed must be within 80-125% of the brand’s levels.
- Device performance: Auto-injectors must require 5-15 Newtons of force to activate. Inhalers must deliver the same dose within ±5%. Failure rates in simulated use must stay below 0.1%.
- Stability and shelf life: Must match the original product under real-world storage conditions.
Where Things Get Tricky: Generic Switching
Here’s the catch: not all generic versions are identical in design. A patient might start on one generic insulin pen, then get switched to another because their pharmacy changed suppliers. The drug inside is the same. But the button feel, the click sound, the way the pen displays the dose-those can differ. For someone with poor eyesight or shaky hands, that’s enough to cause confusion. On PatientsLikeMe, a COPD patient wrote: “Each generic inhaler I got felt different. I had to relearn how to breathe in. I missed doses until my pharmacist sat with me and showed me each one.” This is the biggest risk to compliance with generics: inconsistency. If patients get a different device every few months, they lose confidence. They start doubting whether the new version works as well.
How to Maximize Compliance With Generic Combination Products
The solution isn’t to avoid generics. It’s to manage the transition better.- Train patients on each device. Even a 10-minute demo with a pharmacist can reduce errors by 40%. For complex devices like auto-injectors, 20-30 minutes of hands-on practice is ideal.
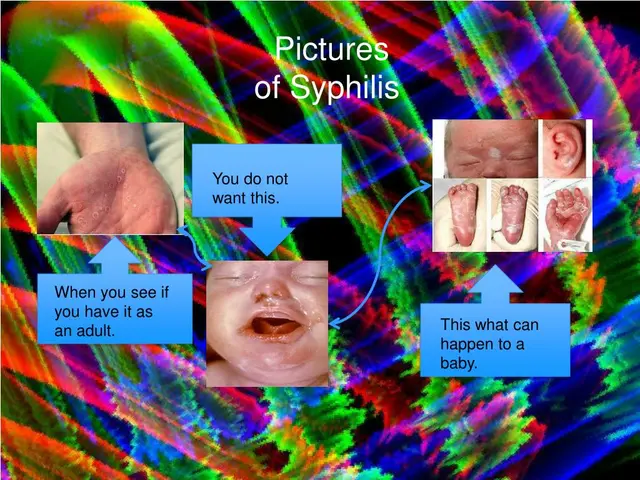
- Use visual aids. Pictures, diagrams, and QR codes linking to short videos help patients remember how to use their device correctly.
- Stick with the same generic when possible. If a patient is doing well on one generic version, don’t switch unless necessary. Consistency matters as much as cost.
- Communicate openly. Tell patients: “This is the same medicine, just a different pen. Here’s how it works.” That simple conversation can boost confidence and adherence by 17-22%.
The Bigger Picture: Why This Matters
Chronic diseases like diabetes, heart failure, and asthma kill millions every year-not because treatments don’t exist, but because people don’t take them as prescribed. Combination products, especially generic ones, are one of the most underused tools in healthcare. They cut costs, simplify routines, and reduce errors. In 2022, the global market for combination products hit $127.5 billion. By 2030, it’s expected to nearly double. And a big chunk of that growth will come from generics. Doctors know this. Sixty-two percent prefer combination products for chronic conditions because they see better adherence in their patients. The challenge now is making sure patients get the same benefit from generics without getting lost in the shuffle.What’s Next?
New FDA guidance released in June 2023 is pushing for clearer rules on how generic combination products can be substituted without confusing patients. Some next-gen generics now include smart features-like Bluetooth-enabled inhalers that track when a dose is taken and send reminders to a phone. These aren’t sci-fi ideas. They’re already in testing. And when they hit the market, they’ll make adherence even easier-especially for older adults and people managing multiple conditions. The goal isn’t just to get people to take their pills. It’s to make taking them feel effortless. Generic combination products are getting us there.Are generic combination products as effective as brand-name ones?
Yes. The FDA requires generic combination products to match the brand in active ingredients, dose accuracy, and device performance. Studies show they work just as well. The only difference is cost-generics are typically 30-80% cheaper.
Can switching between generic versions hurt my adherence?
It can, if the device design changes. Different generics might have different button feels, dose displays, or activation methods. That’s why it’s important to get trained each time you switch and to ask your pharmacist if the new version is the same as the one you used before.
Why do some people distrust generic combination products?
Many people associate generics with lower quality, even though that’s not true. The drug inside is identical. But if the device feels different-like a pen that clicks louder or a patch that sticks differently-it can make patients doubt whether it works. Clear communication and training fix this.
Which conditions benefit most from combination products?
Chronic conditions that require daily, long-term treatment benefit the most. This includes diabetes (insulin pens), high blood pressure (single-pill combos of ACE inhibitors and diuretics), COPD and asthma (inhalers with multiple drugs), and heart disease (drug-eluting stents). These are the areas where adherence drops fastest-and where combination products make the biggest difference.
Will my insurance cover generic combination products?
Almost always. Generic combination products are cheaper, so insurers encourage them. Many plans have lower copays for generics. Some even require you to try a generic before covering the brand-name version. Check your plan’s formulary, but in most cases, you’ll pay less with the generic.






Jarrod Flesch
January 21, 2026 AT 13:52Just had my first generic combo inhaler last week. Same meds, but the click is quieter and the dose counter is bigger. Took me two tries to get used to it, but now I don’t miss doses anymore. Also saved me $120 this month. Aussie here - generics are standard here and nobody bats an eye. 🙌
Ben McKibbin
January 22, 2026 AT 18:57Let’s be real - the pharmaceutical industry doesn’t give a damn about compliance. They want you hooked on brand-name markup. Generic combination products? They’re the quiet revolution nobody wanted to talk about until the bills started piling up. The FDA’s standards are brutal for a reason - if it doesn’t perform identically, it doesn’t get approved. Stop treating generics like knockoffs. They’re engineered clones with better accessibility.
And yes, switching between generics can be a nightmare if your pharmacist doesn’t warn you. But that’s a logistics failure, not a product failure. Fix the supply chain, not the perception.
This isn’t about cheap medicine. It’s about dignity. No one should have to choose between insulin and rent. The real scandal isn’t the generic - it’s that brand-name companies still charge $600 for a pen that costs $12 to make.
Uju Megafu
January 24, 2026 AT 03:28Oh here we go again - the ‘generics are just as good’ propaganda. My cousin in Texas got switched to a generic insulin pen and she had to go to the ER because it didn’t deliver the full dose. She’s lucky she didn’t die. The FDA? They approve based on lab tests, not real people with shaky hands and failing eyesight. And now they want us to trust these ‘same’ pens that look different and feel different? Wake up. This is corporate cost-cutting disguised as healthcare innovation.
And don’t even get me started on how pharmacies switch generics without telling you. That’s not convenience - that’s negligence.
Jerry Rodrigues
January 25, 2026 AT 00:14My grandma’s on a combo pill for BP and cholesterol. She used to forget half her meds. Now she takes one at breakfast. No more pill organizer chaos. She says it feels like magic. I think it’s just good design.
Kelly McRainey Moore
January 25, 2026 AT 05:08I work in a clinic and I’ve seen it firsthand - patients who stopped taking meds because they had 5 different bottles and no idea which one was for what. One pill, one routine, one less thing to stress over. It’s not glamorous, but it saves lives.
Barbara Mahone
January 26, 2026 AT 07:42As someone who grew up in a household where medication adherence was a daily battle, I can say this: the real barrier isn’t understanding - it’s complexity. Combination products strip away the noise. The fact that generics make this accessible to low-income communities isn’t just smart economics - it’s moral. We’ve spent decades framing healthcare as a luxury. This flips that script.
MAHENDRA MEGHWAL
January 26, 2026 AT 17:05It is a matter of profound importance that the regulatory frameworks governing generic combination products remain rigorously consistent with the original branded formulations. The bioequivalence parameters, as stipulated by the FDA, are not merely procedural formalities - they are foundational to patient safety. In the Indian context, where polypharmacy is widespread and literacy barriers persist, the introduction of reliable generics has demonstrably reduced hospitalization rates for chronic conditions. However, the absence of standardized patient education protocols across primary care centers remains a critical gap. Without structured counseling, even the most meticulously engineered device may fail to achieve its intended therapeutic impact.
It is imperative that healthcare systems integrate mandatory device demonstration into every prescription dispensing event. A simple visual aid, coupled with verbal confirmation of understanding, can elevate adherence by more than thirty percent. This is not a technological challenge - it is an organizational one.
Moreover, the phenomenon of generic switching, while economically rational for payers, introduces a hidden cognitive burden upon patients, particularly the elderly. The tactile and auditory cues associated with medical devices become anchors of confidence. Altering these cues without explicit re-education is, in effect, a form of therapeutic disruption.
The global expansion of combination products, particularly in low- and middle-income countries, must be accompanied by robust training infrastructure. Cost reduction without fidelity to patient experience is not progress - it is compromise.
Let us not mistake affordability for adequacy. The goal is not merely to deliver medicine - it is to deliver certainty.
I commend the FDA’s 2023 guidance for its clarity. Yet, implementation remains uneven. The true measure of success lies not in approval rates, but in persistence rates.
Perhaps the next frontier is not in drug formulation, but in human-centered design - devices that speak to the user, not just function for them.
India’s National Health Mission has piloted community health worker-led device training. Early results show a 41% reduction in non-adherence among hypertensive patients. This model deserves global replication.
When we reduce the burden of medication management, we restore agency. And agency, above all, is what enables healing.
Stephen Rock
January 27, 2026 AT 19:09Wow another generic love letter. The FDA approves stuff based on lab rats and not real people. You think your grandma’s pen is the same as the brand? It’s not. The button is softer, the click is different, the display is dimmer. And when you’re 78 and your hands shake? That’s not a minor difference - that’s a death sentence waiting to happen. And don’t even get me started on how pharmacies switch without telling you. This isn’t innovation. It’s corporate greed dressed up as compassion.
Melanie Pearson
January 28, 2026 AT 07:40Ben McKibbin’s post is dangerously naive. The FDA’s standards are a joke. Bioequivalence within 80-125%? That’s a 45% variance. That’s not medicine - that’s gambling. And the device performance metrics? They’re based on ideal conditions, not real-world use by diabetics with neuropathy or COPD patients with arthritis. This isn’t progress. It’s a regulatory loophole exploited by multinational corporations to offload risk onto vulnerable populations. The real problem isn’t the generic - it’s the system that lets them replace brand-name products without mandatory patient retraining. That’s not healthcare. That’s abandonment.
Amber Lane
January 28, 2026 AT 07:51One pill. One routine. One less thing to forget.