Theophylline Interaction Risk Calculator
Theophylline Safety Assessment
Risk Assessment
Clearance Estimate
Calculated clearance rate
Risk Level
Risk level indicator
Key Interactions
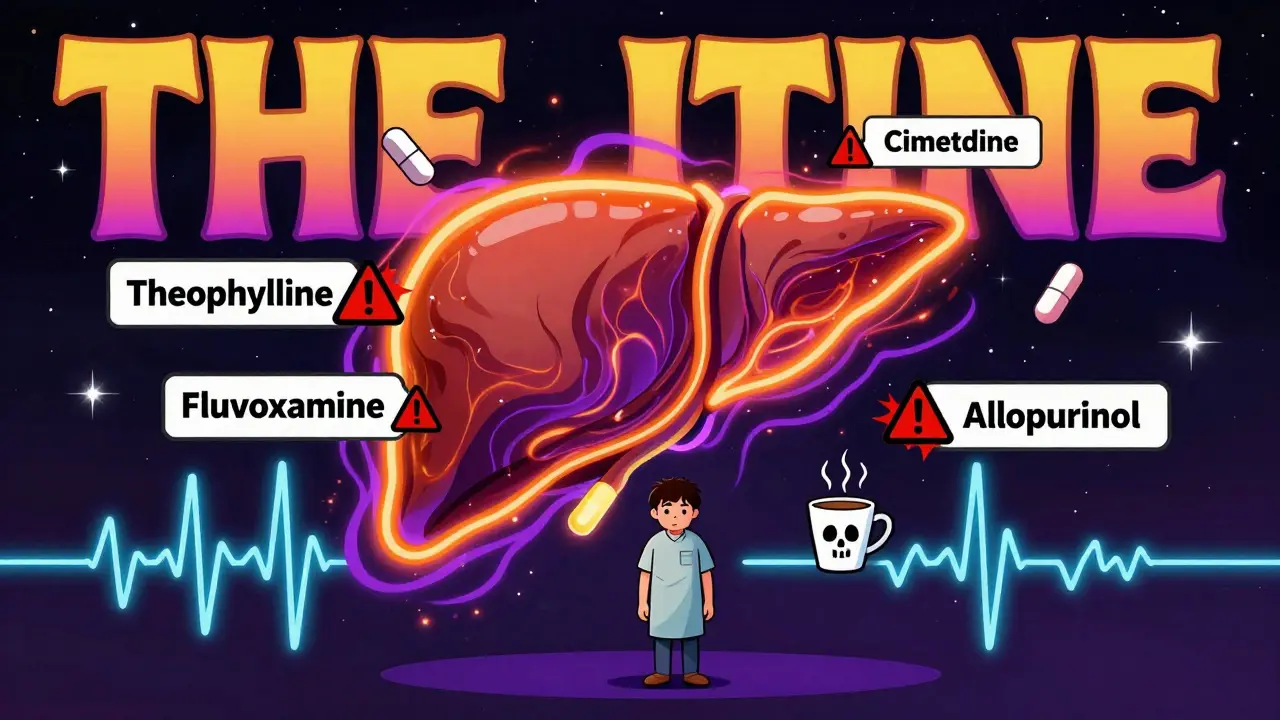
When you take theophylline for asthma or COPD, even a small change in your other meds can turn a safe dose into a dangerous one. This isn’t theoretical - it’s happening in real clinics, emergency rooms, and homes across the country. Theophylline has a razor-thin safety margin: 10 to 20 mcg/mL is the sweet spot. Go above that, and you risk seizures, irregular heartbeats, or worse. And the biggest culprit? Not your dose. It’s what you’re taking with it.
Why Theophylline Is So Fragile
Theophylline doesn’t just float through your body. It’s processed in your liver, mostly by an enzyme called CYP1A2. About 90% of it gets broken down here before leaving your system. That’s why even minor changes to this enzyme can send serum levels skyrocketing. A healthy adult clears theophylline at about 3 liters per hour. But if you’re older, have heart failure, or smoke? That number drops. Now add a medication that blocks CYP1A2, and clearance can plunge by half.Here’s the scary part: theophylline doesn’t follow normal rules. At therapeutic doses, its metabolism becomes non-linear. That means if your clearance drops by 20%, your blood level might jump by 50% or more. A tiny increase in concentration - something you wouldn’t even notice - can push you from safe to toxic without warning.
Medications That Slow Down Theophylline Clearance
Not all drugs are equal when it comes to messing with theophylline. Some barely touch it. Others are landmines.- Fluvoxamine (an SSRI for depression and anxiety): This one cuts clearance by 40-50%. That’s not a suggestion - it’s a red flag. The European Respiratory Society says to avoid combining them entirely. Patients on both have over 12 times higher odds of serious toxicity.
- Cimetidine (an old-school heartburn drug): Reduces clearance by 25-30%. It’s not rare. Many older patients still take it for occasional acid reflux. One case from a community pharmacy showed a patient’s theophylline level jumped from 15.2 to 24.7 mcg/mL in just three days after starting cimetidine. No dose change. Just a pharmacy refill.
- Allopurinol (for gout): Even though it targets a different enzyme (xanthine oxidase), it still interferes with theophylline breakdown. High doses (600 mg/day) reduce clearance by about 20%. Lower doses (300 mg) are safer, but most doctors don’t check the dose when prescribing both.
- Erythromycin and clarithromycin (antibiotics): These macrolides inhibit CYP3A4, which plays a minor role in theophylline metabolism. Still, they can drop clearance by 15-25%. If you’re on theophylline and get pneumonia, don’t assume any antibiotic is safe.
- Furosemide (a water pill): The data is mixed. Some studies show a 10-15% drop in clearance. Others show nothing. But in patients already near the top of the therapeutic range? Even a 10% dip can be enough to trigger symptoms.
What’s worse? Many of these drugs are prescribed without anyone thinking about theophylline. A 2021 study found nearly 30% of patients over 65 on theophylline were also taking at least one of these inhibitors. Only 37% had their dose adjusted.

What Happens When Clearance Drops
The symptoms don’t come slowly. They hit fast.- Nausea, vomiting, stomach pain
- Headache, restlessness, insomnia
- Rapid heartbeat, palpitations
- Shaking or tremors
- Seizures (in severe cases)
These aren’t side effects you can ignore. In 2022, the FDA recorded over 1,800 adverse events tied to theophylline - and 42% of them involved drug interactions. Emergency rooms see about 2,000 cases a year in the U.S. alone. Most are preventable.
One patient I know - a 72-year-old with COPD - was doing fine on 300 mg of theophylline daily. Then he started cimetidine for heartburn. Within a week, he was vomiting, dizzy, and had a heart rate of 130. His theophylline level was 28 mcg/mL. He spent three days in the hospital. His doctor didn’t even know the interaction existed.
Who’s at Highest Risk?
It’s not just about what you take. It’s who you are.- Older adults: Liver function declines with age. Clearance drops naturally.
- People with heart failure: Reduced blood flow to the liver slows metabolism.
- Non-smokers: Smoking boosts CYP1A2. If you quit, your clearance can drop by 30-50% in two weeks - even without new meds.
- Those on multiple drugs: Polypharmacy is the silent killer here. Five meds might be fine. Add one CYP1A2 inhibitor, and the whole system tips.
And here’s the kicker: theophylline use is declining in the U.S., but it’s still common in Asia and Africa. Many patients there rely on it because newer inhalers are too expensive. That means clinicians in these regions are more likely to prescribe it - and less likely to have tools to catch interactions.

How to Stay Safe
If you’re on theophylline, here’s what you need to do:- Know your level. Get a blood test before starting any new medication. Check again 48-72 hours after.
- Never start a new drug without telling your doctor you’re on theophylline. Even OTC meds like antacids or cold pills can matter.
- Ask if your new prescription inhibits CYP1A2. Fluvoxamine, cimetidine, and allopurinol are the big three. If your doctor says it’s fine, ask: “Will this affect how my body breaks down theophylline?”
- If you quit smoking, tell your doctor immediately. Your dose likely needs to go down.
- Watch for symptoms. Nausea, tremors, fast heartbeat - don’t brush them off as “just aging.”
Some clinics now use pharmacist-led programs to monitor theophylline patients. One study showed hospitalizations dropped by 37% when pharmacists reviewed all meds every 30 days. That’s not magic. That’s just paying attention.
The Bigger Picture
Theophylline isn’t going away. It’s cheap. It works. And in places where inhalers cost more than a week’s groceries, it’s still the only option. But its use is shrinking in places like the U.S., where newer drugs dominate. That creates a dangerous blind spot: younger doctors never learned how to manage it. Older patients keep taking it. And the interactions? They’re still there.The American Thoracic Society now lists “optimizing theophylline use in polypharmacy” as a top research priority. That’s code for: we’re still losing people to this. And it’s not because the drug is bad. It’s because we’re not paying attention to the details.
There’s a reason the FDA calls theophylline a “sensitive substrate” of CYP1A2. It’s not just sensitive. It’s fragile. And if you’re on it, you need to treat it like a live wire - respect it, monitor it, and never assume another drug is harmless.
Can I take ibuprofen with theophylline?
Yes, ibuprofen does not significantly affect theophylline metabolism. It doesn’t inhibit CYP1A2 or CYP3A4 in a clinically meaningful way. You can safely take ibuprofen for pain or inflammation while on theophylline. But always check with your pharmacist or doctor before starting any new medication, even over-the-counter ones.
Does coffee affect theophylline levels?
Caffeine is chemically similar to theophylline and is also metabolized by CYP1A2. Heavy coffee consumption (4+ cups daily) can slightly increase theophylline clearance, potentially lowering its effectiveness. On the flip side, if you suddenly cut out coffee, your theophylline levels could rise - similar to quitting smoking. Consistency matters. Don’t change your caffeine intake without telling your doctor.
How often should theophylline levels be checked?
When you first start theophylline, check levels after 3-5 days. After that, check every 6-12 months if stable. But anytime you start or stop a new medication - especially antibiotics, heartburn drugs, or antidepressants - get a level checked within 48-72 hours. Also check after quitting smoking or if you develop heart failure or liver issues.
Is theophylline still used today?
Yes, but less often. In the U.S., its use has dropped by 62% since 2000. But it’s still used for refractory asthma, nocturnal COPD symptoms, and in regions where newer inhalers are unaffordable. Global use is higher in Asia and Africa, where it makes up over 10% of COPD treatment. It’s not first-line anymore - but when it’s needed, it works.
Can I switch to a different medication to avoid these interactions?
Absolutely. Long-acting beta-agonists (like salmeterol or formoterol) and inhaled corticosteroids are now preferred for most patients. They’re safer, more effective, and don’t have dangerous drug interactions. If you’re on theophylline and taking multiple other meds, talk to your doctor about switching. The risk of interactions may outweigh the benefit - especially if you’re over 65 or on more than five medications.





Swapneel Mehta
December 21, 2025 AT 15:04Theophylline is one of those drugs that feels like a relic from the 80s, but it still saves lives where inhalers are unaffordable. I’ve seen patients in rural India on it for decades - no fancy monitoring, just a pill and a prayer. But this post? Exactly why we need better education for community pharmacists and frontline doctors. It’s not the drug’s fault. It’s the system ignoring the details.
Dan Adkins
December 22, 2025 AT 12:05It is imperative to underscore the clinical significance of cytochrome P450 enzyme modulation in the context of narrow therapeutic index medications. Theophylline, as a prototypical substrate of CYP1A2, exhibits pharmacokinetic nonlinearity that renders even minor pharmacodynamic perturbations clinically consequential. The cited pharmacokinetic alterations induced by fluvoxamine and cimetidine are not merely statistical anomalies - they represent tangible, life-threatening deviations from homeostasis.
Moreover, the assertion that ‘many doctors don’t know’ is not an indictment of individual practitioners, but rather a systemic failure in pharmacovigilance infrastructure. In jurisdictions where electronic health records lack automated interaction alerts, such adverse events are not merely possible - they are inevitable.
It is therefore recommended that all institutions prescribing theophylline implement mandatory CYP1A2 interaction screening protocols, ideally integrated into e-prescribing systems. Until then, the burden of safety remains disproportionately on the patient - an ethically untenable paradigm.
Orlando Marquez Jr
December 24, 2025 AT 02:32As someone who’s worked in respiratory care in both urban US clinics and rural outreach programs, I’ve seen this play out too many times. Theophylline isn’t glamorous, but it’s reliable. In places where a Nebulizer costs more than a month’s rent, this pill is the difference between breathing and not breathing. But you’re right - no one talks about the interactions. We teach new residents about albuterol and Advair, but theophylline? It’s treated like a footnote. That’s not just negligence - it’s a gap in training that’s costing lives.
Cameron Hoover
December 25, 2025 AT 23:07I used to think theophylline was just an old-school asthma drug. Then my uncle ended up in the ER after taking cimetidine for heartburn. He was fine for years - then one day, he couldn’t stop shaking. His level was 29. They didn’t even connect it until his daughter mentioned the new pill. He spent three days in ICU. I didn’t know something so common could be a silent killer. Now I check every single new med with his pharmacist. This post? It’s terrifying. But it’s also the kind of info that saves lives if it spreads.
mukesh matav
December 26, 2025 AT 05:08My dad’s on theophylline. He quit smoking two years ago. We didn’t tell his doctor. He started getting dizzy. We thought it was aging. Turns out his levels doubled. He’s been stable since they cut his dose. I’m glad this got posted. Most people don’t realize quitting smoking affects meds like this. It’s not just about lungs - it’s about liver enzymes. That’s wild.
Peggy Adams
December 27, 2025 AT 21:55So… is this just Big Pharma hiding that theophylline is dangerous so they can sell you expensive inhalers? Because I’ve read that the FDA knew about these interactions for decades and still let it stay on the market. And now they’re pushing ‘newer’ drugs that cost 10x more. Coincidence? I think not.
Sarah Williams
December 29, 2025 AT 01:12This is exactly why I always ask my pharmacist about every new pill - even ibuprofen. I’m on theophylline and three other meds. One wrong combo and I could be in the hospital. I don’t trust doctors to catch everything. My pharmacist did. She flagged cimetidine for me before I even got the script. That’s the kind of care we need more of.
Jay lawch
December 29, 2025 AT 05:09Let’s be honest - theophylline is a relic of colonial medicine. Developed in the West, used in the Global South because the West doesn’t want to fund affordable alternatives. The fact that it’s still in use in India and Nigeria isn’t a testament to its efficacy - it’s a symptom of economic exploitation. We’re told to ‘manage’ this drug, but no one asks why we’re still stuck with it. The real issue isn’t CYP1A2 - it’s the global health inequality that forces people to risk their lives on 70-year-old pills while Westerners get sleek inhalers. This isn’t a medical problem. It’s a moral one.
And don’t get me started on how Western doctors ignore this because they think ‘it’s not common here.’ Out of sight, out of mind. Until it’s your uncle in a Nigerian village dying because his doctor didn’t know about cimetidine. Then it’s too late.
Christina Weber
December 30, 2025 AT 05:39There is a critical grammatical error in the post: the phrase 'it’s what you’re taking with it' lacks proper punctuation and is colloquially imprecise. It should read: 'It is not your dose - it is what you are taking in conjunction with it.' Furthermore, the use of 'razor-thin' as a descriptor, while evocative, is nonstandard in clinical literature and undermines the post’s credibility. Theophylline’s therapeutic index is not 'razor-thin' - it is narrow, quantifiable, and well-documented. Precision in language matters, especially when lives are at stake. This post is medically accurate in substance, but its informal tone risks diminishing its authority among clinicians who rely on rigorous documentation.
Erika Putri Aldana
December 30, 2025 AT 21:23