What Pulmonary Long COVID Really Is
When you hear 'long COVID,' you might think of fatigue or brain fog. But for many survivors, the real battle happens in the lungs. Pulmonary long COVID affects roughly one-third of all long COVID cases, according to 2025 research from the Centre for Heart Lung Innovation. This condition isn't just about lingering coughs-it's a complex inflammatory process that damages the lungs' smallest airways long after the virus is gone. About 12.6% of hospitalized patients develop permanent lung scarring called post-COVID pulmonary fibrosis (PCPF), and 30.4% still struggle with breathing three months after discharge.
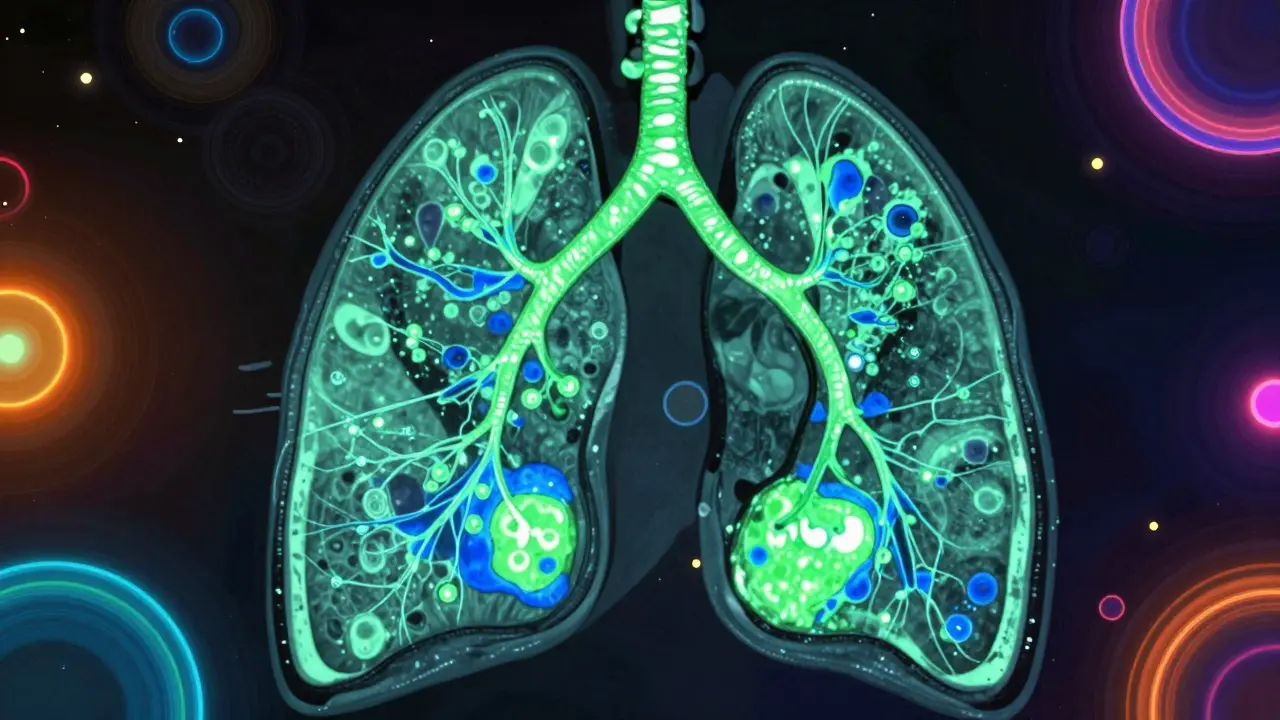
The Hidden Damage in Your Lungs
Traditional scans like chest X-rays or CTs often look normal, but that doesn't mean your lungs are fine. Advanced imaging with hyperpolarized xenon MRIAn advanced imaging technique that visualizes oxygen transfer in the lungs' smallest airways where traditional scans fail. reveals what's really happening. This technology shows how oxygen moves through tiny air sacs, exposing problems invisible to standard tests.
Researchers at the University of British Columbia's Heart Lung Innovation Centre discovered something shocking: neutrophils-immune cells that normally fight infection-keep triggering inflammation even after the virus is gone. They act like 'dirty bombs' in the lungs' smallest airways, causing lasting damage. This neutrophilic inflammation explains why many patients feel breathless during simple tasks like climbing stairs or carrying groceries.
Why Standard Tests Miss the Problem
Doctors often rely on spirometry tests measuring FEV1 (Forced Expiratory Volume in 1 second), but these can show normal results while patients still struggle. A 2025 study in the International Journal of Chronic Obstructive Pulmonary Disease found hospitalized patients had significantly lower FEV1 measurements (2.03 ± 0.60 L) compared to outpatients (2.56 ± 0.72 L), yet many still felt fine during routine checkups.
The mMRC dyspnea scaleA tool measuring breathlessness severity during daily activities, where scores ≥2 indicate significant respiratory dysfunction. provides better insight. Patients scoring 2 or higher on this scale at one month post-infection are 1.49 times more likely to have persistent breathing issues. This simple questionnaire helps doctors spot problems early when standard tests say everything's normal.

How Rehabilitation Programs Help
Specialized pulmonary rehabilitation isn't just for COPD patients-it's crucial for long COVID lung recovery. Programs typically start 4 weeks after acute infection and last 8-12 weeks with sessions 2-3 times weekly. These multidisciplinary programs combine breathing exercises, aerobic training, and strength work tailored to individual limitations.
For example, diaphragmatic breathing teaches patients to use their diaphragm properly instead of shallow chest breathing. Pursed-lip breathing helps keep airways open longer during exhalation. A 2025 Lung Foundation Australia review found patients who completed full programs saw measurable improvements in FEV1 and diffusion capacity, along with better 6-minute walk distance results. One participant, a 45-year-old teacher, went from struggling to walk 100 meters without stopping to completing her daily commute without breathlessness within 10 weeks.
Special Considerations for Pre-existing Conditions
People with existing lung conditions face higher risks. Those with COPD who catch COVID-19 have 4.6% higher mortality rates and experience twice as many acute exacerbations compared to non-COVID COPD patients. Their rehabilitation requires extra caution-doctors monitor heart function closely since 20% of hospitalized COPD patients develop heart failure complications.
Medications also play a role. The Korean study of 688 patients found remdesivir use was linked to reduced PCPF risk, while baricitinib increased risk. However, researchers noted this might reflect underlying patient differences rather than direct cause-effect. Always discuss medication choices with your doctor before making changes.

What's Next in Research
The RECOVER InitiativeA major NIH-funded research program tracking long COVID's impact across multiple body systems. is leading new studies. Their September 2025 update highlighted connections between pulmonary complications and kidney disease, with a 1.65 hazard ratio for chronic kidney disease in long COVID patients. Clinical trials testing neutrophil-targeted therapies are underway, building on the discovery that persistent neutrophil activity drives lung damage.
Hyperpolarized xenon MRI is expanding beyond research labs. Duke University and University of Kansas Medical Center are now using it clinically to track treatment responses. Early data from these centers shows promise for personalized rehab plans based on individual lung function patterns. While 12.6% of hospitalized patients develop permanent fibrosis, most see gradual improvement over six months with proper care.
Frequently Asked Questions
Can standard lung tests detect pulmonary long COVID?
No. Traditional tests like chest X-rays, CT scans, and spirometry often show normal results even when patients struggle with breathing. Hyperpolarized xenon MRI reveals gas exchange issues in small airways that standard tests miss. Doctors now use the mMRC dyspnea scale to assess breathlessness severity during daily activities.
How long does pulmonary rehabilitation take?
Most programs last 8-12 weeks with sessions 2-3 times weekly. Improvements in lung function and daily activities typically appear within 4-6 weeks. Patients with pre-existing conditions like COPD may need longer programs with closer monitoring.
Are there specific exercises for lung recovery?
Yes. Diaphragmatic breathing (using the diaphragm instead of chest muscles), pursed-lip breathing (inhaling through nose, exhaling slowly through pursed lips), and gentle aerobic activities like walking or cycling are common. Physical therapists customize these based on individual limitations and goals.
Does vaccination affect long-term lung effects?
Current data suggests vaccinated individuals have lower risks of severe lung complications. A 2025 study in the European Respiratory Journal found fully vaccinated patients were 40% less likely to develop persistent respiratory symptoms compared to unvaccinated counterparts. However, breakthrough cases can still cause pulmonary long COVID, especially in immunocompromised people.
When should I see a specialist for lung issues?
See a pulmonologist if you experience ongoing shortness of breath during light activities, chest pain, or persistent cough after 4 weeks. Early intervention improves outcomes-don't wait until symptoms worsen. Your primary care doctor can refer you to a rehabilitation specialist if needed.






Andre Shaw
February 5, 2026 AT 20:22Hold up, this article's got it all wrong.
Pulmonary long COVID is just a myth pushed by the medical industry to sell expensive tests.
My uncle had COVID and his lungs were fine-no scarring, no issues.
They're just trying to scare people into paying for unnecessary procedures.
Hyperpolarized xenon MRI? That's a scam.
Stick to basic breathing exercises and you'll be golden.
This whole thing's a cash grab.
The research from the Centre for Heart Lung Innovation is probably funded by pharmaceutical companies looking to profit.
They're cherry-picking data to make it seem like there's a crisis.
In reality, most people recover naturally without any special treatment.
The real problem is doctors overdiagnosing and creating unnecessary panic.
I've read studies showing that the majority of 'long COVID' symptoms are psychosomatic.
It's all in their heads.
The medical industry is in cahoots with insurance companies to push expensive tests.
Don't fall for it-trust your body.
If you're not hospitalized, you're probably fine.
This is all just a way for hospitals to make money.
They're using scare tactics to get people to pay for treatments they don't need.
The science is being manipulated.
Wake up, people!
Tehya Wilson
February 5, 2026 AT 23:15The data presented is insufficient to support the claims made Further research is needed before drawing conclusions
jan civil
February 6, 2026 AT 15:23Interesting findings on neutrophil activity. It's crucial to consider how this affects rehabilitation strategies. More research could help tailor treatments better.
Joyce cuypers
February 6, 2026 AT 23:51I agree that more research is needed. But the current data on neutrophil activity is promising. Diahphragmatic breathing exercises can help many patients. It's important to stay hopeful and consistent with rehab. Also, check out online resources for proper technique. Every little bit helps.
Lisa Scott
February 7, 2026 AT 01:22This is all a scam. The government and Big Pharma are using this to push experimental treatments. Neutrophils aren't the issue-it's the vaccines. The real damage comes from mRNA tech. They're hiding the truth. Always question the source. The studies cited are funded by the same companies. They're cherry-picking data. The real issue is vaccine-induced autoimmunity. The medical community is covering it up. Don't trust the mainstream media. The truth is out there.
Katharine Meiler
February 8, 2026 AT 17:21The study's methodology is sound regarding neutrophilic inflammation. However, the clinical application of hyperpolarized xenon MRI requires further validation. Standard spirometry remains a useful tool despite limitations. A multidisciplinary approach is essential for effective rehabilitation protocols. The data supports the importance of early intervention. More research is needed to establish standardized treatment guidelines.
Laissa Peixoto
February 8, 2026 AT 21:18It's important to critically evaluate sources. The immune system's complexity means there's no single villain. Perhaps the answer lies in understanding the body's natural healing processes rather than blaming specific entities. This raises questions about the nature of chronic illness and the mind-body connection. We must approach healthcare holistically.
lance black
February 9, 2026 AT 11:20Keep pushing through the rehab. You've got this!
Albert Lua
February 10, 2026 AT 11:53In my country, we have similar challenges with post-viral lung issues. The key is community support and tailored exercises. Let's share experiences to help each other.
Thorben Westerhuys
February 12, 2026 AT 07:34This is so important! The neutrophil issue is critical-so many people don't realize it! But wait, what about the kidney connection? It's all so complex... I need to read more! The research is evolving rapidly. Stay informed!
Lana Younis
February 12, 2026 AT 12:45Great info on the mMRC scale! I've seen patients benefit from it. Just remember, everyone's different-what works for one might not for another. Keep those rehab sessions consistent, even if it's slow progress. Dyspneea is a common symptom but manageable with the right approach.