Elderberry & Immunosuppressants Interaction Checker
Check Elderberry Safety with Your Medication
This tool helps you understand potential interactions between elderberry and your immunosuppressant medication. Always consult your healthcare provider before making changes to your treatment.
Every winter, people reach for elderberry syrup, gummies, or capsules hoping to dodge the flu. It’s popular, natural, and many swear by it. But if you’re on immunosuppressants-medications that quiet your immune system after a transplant or for autoimmune diseases-elderberry might be doing the opposite of what you need. It’s not just a harmless herbal boost. It could be quietly undermining your treatment.
Why Elderberry Is a Double-Edged Sword
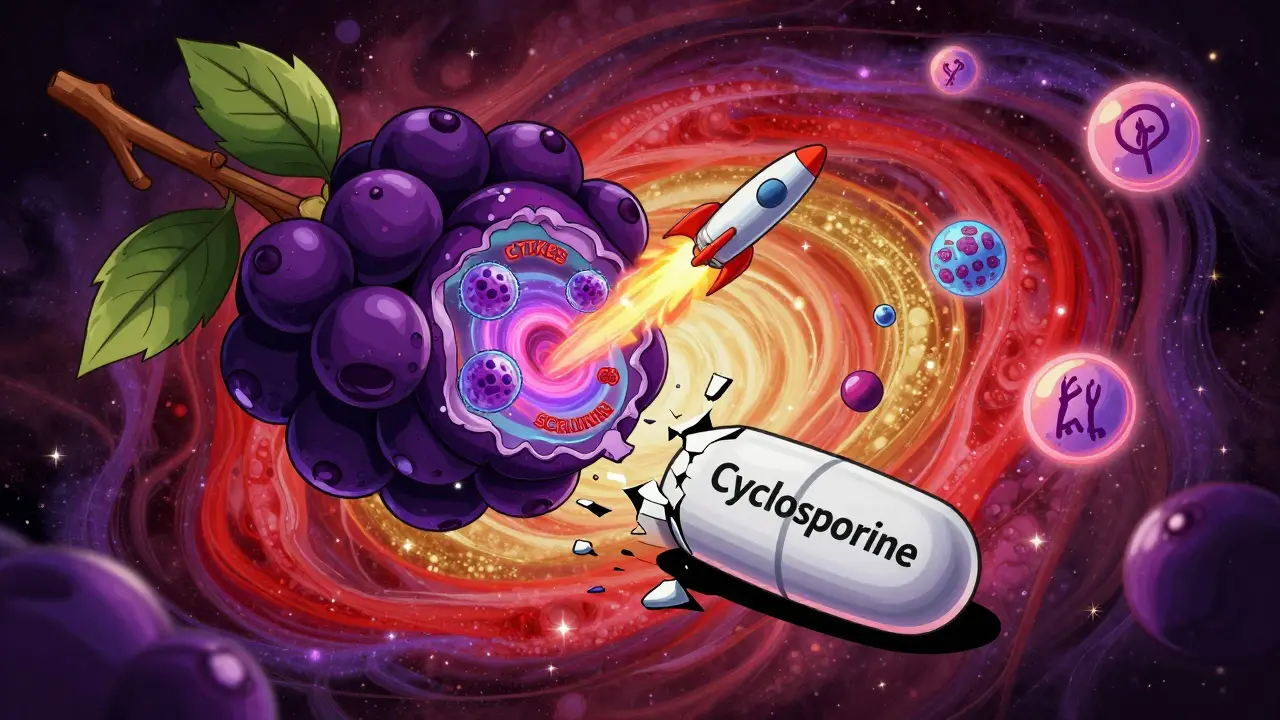
Elderberry comes from the black elder tree (Sambucus nigra). For centuries, it’s been used in teas and syrups to fight colds and flu. Modern studies back this up: one 2016 trial with 312 air travelers showed it cut cold duration by 3 to 4 days. That’s impressive-if your immune system is working fine. But here’s the catch: elderberry doesn’t just help your body fight viruses. It actively turns up the volume on your immune response. Its key compounds-anthocyanins, flavonols, and phenolic acids-trigger immune cells to release more cytokines, interleukins, and tumor necrosis factor. These are the chemical signals that tell your body to attack invaders. Sounds good, right? Not if you’re on immunosuppressants. Drugs like cyclosporine, tacrolimus, mycophenolate, and prednisone work by dialing down those same signals. They’re designed to stop your immune system from attacking your new organ or your own joints. If elderberry is turning those signals back up, you’re fighting your own medication. That’s not just risky-it’s dangerous.Which Immunosuppressants Are Most at Risk?
Not all immunosuppressants react the same way, but the biggest red flags are with drugs that target specific immune pathways:- Cyclosporine (Neoral, Sandimmune) and tacrolimus (Prograf): These calcineurin inhibitors are common after organ transplants. Elderberry may lower their blood levels, making rejection more likely.
- Mycophenolate (CellCept): Used for lupus, kidney disease, and transplants. Elderberry’s cytokine boost can counteract its suppression.
- Azathioprine (Imuran) and prednisone: Even broad-acting drugs like these can be disrupted by elderberry’s targeted immune stimulation.
- Biologics like infliximab (Remicade): These target specific inflammation pathways. Elderberry’s effect on tumor necrosis factor may interfere directly.
The Controversy: Is the Risk Real or Just Theoretical?
You might see headlines saying, “Elderberry is safe-even for immunosuppressed patients.” That’s based on a 2021 PubMed review that found no evidence elderberry “overstimulates” the immune system. But here’s the problem: that study looked at healthy people with colds, not people on immunosuppressants. The CSIRO Publishing review from 2021, backed by the Royal New Zealand College of General Practitioners, took a different view. They explicitly warned that elderberry “may increase cytokines and interfere with the effectiveness of immunosuppressants.” That’s not speculation-it’s based on lab studies showing up to a 30% increase in interleukin-6 and TNF-alpha in immune cells exposed to elderberry extract. Then there’s the patient experience. On forums like the American Autoimmune Related Diseases Association, some say they’ve taken elderberry for years on CellCept with no issues. Others report flare-ups of lupus or ulcerative colitis right after starting it. Anecdotes aren’t proof-but when 87% of 142 forum posts warn against it, it’s worth listening. The truth? We don’t have large-scale clinical trials proving elderberry causes rejection or flare-ups in humans. But we have enough biological plausibility, case reports, and expert consensus to treat this as a real risk.
What Do Experts Actually Recommend?
The advice from major medical groups is clear:- Organ transplant recipients: Avoid elderberry completely. Sweet’s Elderberry Safety Guide (2023) says bluntly: “Anyone who has received an organ transplant should avoid elderberry.”
- Autoimmune disease patients: It depends. Rheumatologists often say no during active disease (like a lupus flare or RA flare-up), but might allow it in remission-though rarely. The Arthritis Foundation’s 2023 update says: “If you’re taking medication for rheumatoid arthritis, lupus, multiple sclerosis, or Hashimoto’s thyroiditis, it’s best to skip elderberry.”
- Anyone unsure: Talk to your doctor or pharmacist before taking it. Don’t assume it’s safe because it’s “natural.”
What Can You Take Instead?
If you’re immunosuppressed and want to support your immune system without risking your meds, here are safer options:- Vitamin D: Supports immune regulation without triggering cytokine storms. A 2022 survey of 150 rheumatologists showed 78% preferred recommending vitamin D over elderberry.
- Zinc: Helps with cold recovery, but doesn’t activate immune pathways the way elderberry does.
- Probiotics: Especially strains like Lactobacillus rhamnosus and Bifidobacterium lactis, which support gut immunity without systemic inflammation.
- Good sleep and stress management: These are the most powerful, evidence-backed immune supports you already have access to.
The Bigger Picture: Why This Matters Now
The global elderberry market hit $1.27 billion in 2022 and is expected to grow past $2 billion by 2028. Meanwhile, about 3.1 million Americans take immunosuppressants for autoimmune diseases, and another 200,000 live with organ transplants. That’s a huge overlap of people who might be taking elderberry without knowing the risk. The FDA doesn’t require supplement labels to warn about drug interactions. The European Medicines Agency did issue a warning in 2021-but the U.S. hasn’t. That leaves consumers in the dark. New research is underway. The NIH launched a Phase II trial in January 2023 (NCT05213456) to measure how elderberry affects tacrolimus levels in kidney transplant patients. Results are expected in late 2024. Until then, caution is the only reliable guide.What to Do Right Now
If you’re on immunosuppressants:- Check your supplement bottles. Look for elderberry extract, Sambucus nigra, or black elderberry.
- Stop taking it if you’re unsure. It’s not worth the risk.
- Talk to your doctor or pharmacist. Bring your supplement list to your next appointment.
- Replace it with vitamin D or another safer option.
Supplements aren’t harmless. Just because something is plant-based doesn’t mean it’s safe with your meds. Elderberry is a perfect example: helpful for some, dangerous for others. Knowing the difference could mean the difference between a quick recovery and a hospital visit.
Can I take elderberry if I’m on prednisone?
It’s not recommended. Prednisone suppresses inflammation by reducing cytokine activity. Elderberry increases those same cytokines, which can make prednisone less effective. Even if you feel fine, this interaction can quietly raise your risk of flare-ups or organ rejection. Talk to your doctor before combining them.
Does elderberry affect blood pressure or blood sugar?
Yes, elderberry may lower blood sugar and blood pressure slightly. If you’re on medications for diabetes or hypertension, combining it with elderberry could cause levels to drop too low. This adds another layer of risk beyond immune interactions. Always check with your provider if you’re on any daily medications.
Is elderberry syrup safer than capsules?
No. Both forms contain the same active compounds-anthocyanins and flavonoids-that trigger immune activity. The risk isn’t about the delivery method, but the dose and concentration. A tablespoon of syrup can contain 300mg or more of standardized extract-the level linked to immune stimulation. Always assume both are risky if you’re immunosuppressed.
What happens if I accidentally take elderberry while on immunosuppressants?
One dose is unlikely to cause immediate harm, but it can disrupt your drug levels over time. If you’ve taken it once, stop immediately and monitor for signs of rejection or flare-ups-fever, fatigue, joint pain, swelling, or unusual bruising. Contact your doctor and ask for a blood test to check your drug levels. Don’t wait for symptoms to appear.
Are there any supplements that are safe to take with immunosuppressants?
Yes. Vitamin D, zinc (in moderate doses), and certain probiotics like Lactobacillus and Bifidobacterium strains are generally considered safe and don’t interfere with immune-suppressing drugs. Always confirm with your care team, but these are better alternatives to elderberry, echinacea, or astragalus, which all carry interaction risks.





TONY ADAMS
January 26, 2026 AT 13:44bro just stop taking that elderberry crap if you’re on meds. i saw my cousin go into the hospital because he thought ‘natural’ meant ‘safe.’ dumbass.
Ashley Karanja
January 27, 2026 AT 14:11There’s a profound epistemological tension here between anecdotal lived experience and pharmacological mechanism. While individual patients may report no adverse effects from concurrent elderberry use, the cytokine modulation profile of Sambucus nigra-specifically its upregulation of IL-6, TNF-alpha, and interferon-gamma pathways-creates a biologically plausible, if not statistically quantified, risk for pharmacodynamic antagonism with calcineurin inhibitors and mTOR suppressants. The absence of RCTs doesn’t negate the convergence of in vitro evidence, case reports, and clinical intuition. We must resist the temptation to equate ‘no proof of harm’ with ‘proof of safety.’
Karen Droege
January 28, 2026 AT 15:15Oh my god. I’ve been taking elderberry syrup every winter since my kidney transplant in 2018. I thought it was helping me stay healthy. I just checked my bottle-‘Black Elderberry Extract 400mg per tsp.’ I’m deleting it from my shelf right now. I’m so mad at myself for ignoring the red flags. Thank you for writing this. I’m telling my entire transplant group about this.
Napoleon Huere
January 30, 2026 AT 03:49Here’s the thing nobody talks about: we’re not just talking about a supplement. We’re talking about a cultural myth. We’ve been sold this idea that plants are inherently good, that science is corporate and cold, and that ‘natural’ is a moral good. But elderberry? It’s a potent phytochemical cocktail. It doesn’t care if you’ve got a new liver. It just fires up your immune cells like they’re at a rave. And if your meds are trying to put out that fire? You’re not ‘boosting immunity’-you’re playing Russian roulette with your transplant.
Patrick Merrell
January 30, 2026 AT 20:24People like you who say ‘just avoid it’ are the reason we have a public health crisis. You don’t know the full story. My rheumatologist said I could take it in moderation. I’ve been on CellCept for 7 years. I’ve had zero flares. You’re scaring people with fear, not facts.
George Rahn
January 31, 2026 AT 09:20Let us not forget: the American ethos of self-medication has birthed a generation of pharmacological anarchists. We fetishize the botanical while demonizing the pharmaceutical, as if nature’s pharmacy is somehow untainted by the same chemical laws that govern the lab. Elderberry is not a benign tea-it is a molecular saboteur. To equate its use with ‘wellness’ is to misunderstand the very nature of immunosuppression: it is not suppression of vitality, but the deliberate restraint of self-destruction. To disrupt that restraint with a berry is not wisdom-it is hubris dressed in herbal garb.
Shweta Deshpande
February 1, 2026 AT 22:06I’m so glad someone finally wrote this. My mom has lupus and she was taking elderberry because her friend’s cousin swore by it. I printed out this whole article and left it on her kitchen counter with a sticky note: ‘Love you, please don’t risk it.’ She cried and said she’ll stop. I just wish more people had this info before they started. You’re not being dramatic-you’re being lifesaving.
Neil Thorogood
February 2, 2026 AT 18:01So let me get this straight… you’re telling me that the one thing I’ve been using to avoid sick days for 10 years… is secretly trying to kill my transplant? 🤡 I feel like I’ve been lied to by every wellness influencer on Instagram. Time to throw my elderberry syrup in the trash and start taking vitamin D like a grown-up. 💪
Jessica Knuteson
February 3, 2026 AT 06:52Studies show correlation not causation. Anecdotes aren’t data. You’re fearmongering. I’m still taking it.
Robin Van Emous
February 3, 2026 AT 17:34I appreciate how this post lays out the science without shaming people who’ve taken elderberry. I’m from a culture where herbal remedies are sacred, and it’s hard to tell someone to stop something their grandma swore by. But if this could prevent even one person from losing their transplant, it’s worth the discomfort. I’ve shared this with my family, my book club, and my pharmacist. Knowledge is the real medicine here.