Esketamine Blood Pressure Safety Calculator
Blood Pressure Screening Guide
Esketamine nasal spray (Spravato) requires strict blood pressure monitoring due to potential spikes. Your blood pressure must be below 160/100 mmHg at screening time to qualify for treatment. This tool helps you understand if your readings meet the clinical criteria.
Enter your blood pressure values to see if you qualify for esketamine treatment.
What Esketamine Nasal Spray Actually Does to Your Body
If you’ve been told you might be a candidate for esketamine nasal spray - brand name Spravato - you’re probably wondering what really happens when you use it. This isn’t another antidepressant you pop in the morning with coffee. It’s a fast-acting, FDA-approved treatment for treatment-resistant depression, but it comes with a set of intense, short-term side effects that require strict medical supervision. You don’t just walk into a clinic, get a spray, and leave. You’re monitored for two full hours after each dose. Why? Because esketamine doesn’t just lift your mood - it temporarily changes how your brain and body work.
Unlike SSRIs or SNRIs that work on serotonin or norepinephrine, esketamine targets the glutamate system. It blocks NMDA receptors, which are like gatekeepers for a key brain signaling pathway. This triggers a cascade of neural activity that can lift depression symptoms within hours - not weeks. But that same mechanism is what causes dissociation and spikes in blood pressure. These aren’t rare side effects. They’re expected. And they’re managed on purpose.
Dissociation: It’s Not Just ‘Feeling Weird’
Dissociation is the most common side effect of esketamine. In clinical trials, more than half of patients (56%) reported feeling detached from themselves or their surroundings. That’s not a fluke. It’s built into how the drug works.
People describe it in different ways: feeling like you’re watching yourself from outside your body, time slowing down, colors seeming brighter or distorted, or even hearing sounds as if they’re underwater. Some report mild confusion. A small number - about 6% - experience severe dissociation, where the feeling becomes overwhelming. But here’s the key: it doesn’t last. Peak effects happen around 40 minutes after the spray, and by 90 minutes, most people are back to normal. By two hours, nearly everyone is clear-headed again.
It’s not hallucinations in the psychotic sense. It’s more like a deep, temporary shift in perception. And yes, it happens more often with the higher 84 mg dose than the 56 mg. That’s why doctors start low. Many patients say the first few treatments are the hardest. By the third or fourth session, the dissociation feels less intense - sometimes barely noticeable. One user on Reddit said, ‘My first time felt like I was floating through a dream. By the fourth, I just sat there and listened to music.’
Clinics are trained to handle this. They dim the lights, play calm music, and avoid talking too much during the session. You’re not alone - a nurse is right there, checking in. If things get too intense, they can give you a small dose of a benzodiazepine like lorazepam. But that’s rare. Less than 2% of treatments require it.
Why Your Blood Pressure Rises - And Why That Matters
Right after you use the spray, your blood pressure goes up. Not a little. On average, systolic pressure jumps 14 to 23 mmHg. Diastolic can rise by 7 to 16 mmHg. That’s enough to trigger a warning in most clinics.
This isn’t anxiety. It’s a direct effect of the drug on your autonomic nervous system. The spike starts within 5 minutes, peaks at 40 minutes, and drops back to normal within 90 to 120 minutes. In clinical trials, about 33% of users had blood pressure readings above 140/90 - the clinical threshold for hypertension. Only 14% of placebo users did.
For most people, this is harmless. But if you have uncontrolled high blood pressure, heart disease, or a history of aneurysms, esketamine is off-limits. Screening is strict. Before each treatment, your blood pressure is checked. If it’s over 160/100, they won’t give you the spray. You’ll need to get it under control first.
One patient with hypertension shared on PatientsLikeMe: ‘I had to stop after two sessions. My systolic hit 170 even though I’m on meds.’ That’s why monitoring isn’t optional. Nurses check your blood pressure every 5 to 10 minutes during the first hour, then every 15 to 30 minutes after that. They’re watching for red flags - not just numbers, but symptoms like headache, chest pain, or dizziness. If something looks off, they stop the session and treat it immediately.
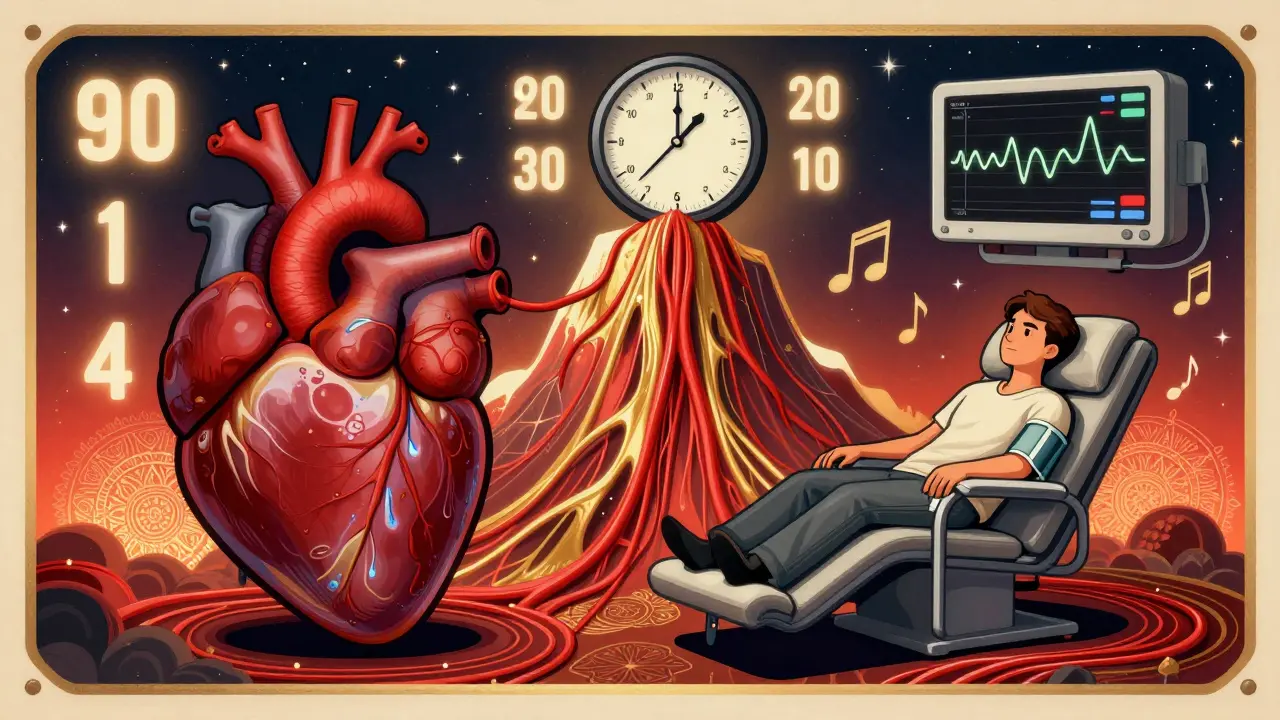
The Two-Hour Monitoring Rule: Why It’s Non-Negotiable
You can’t take esketamine home. You can’t use it in your doctor’s office unless they’re certified under the FDA’s REMS program. That stands for Risk Evaluation and Mitigation Strategy - a safety system designed specifically for drugs with serious, short-term risks.
Here’s what REMS requires:
- You must be in a certified clinic - not a regular mental health office.
- You must self-administer the spray under direct supervision.
- You must be monitored for at least two hours after each dose.
- Your vital signs (blood pressure, heart rate, oxygen) are checked repeatedly.
- You’re assessed for dissociation using a standardized scale (CADSS) at the 40-minute mark.
- You must sign a Patient-Provider Agreement before every session.
This isn’t bureaucracy. It’s life-saving structure. In 2022, a survey of 147 certified centers found that 95% strictly followed the two-hour rule. Only 5% ever let someone leave early - and only after confirming stable vitals and minimal side effects.
Setting up a Spravato clinic costs around $18,500 on average - for private rooms, monitoring equipment, oxygen tanks, and staff training. Clinics need to be ready for anything: a sudden drop in oxygen, a seizure, a panic attack. That’s why you won’t find this treatment in rural areas as easily as in cities. There are only 0.8 certified centers per 100,000 people in rural U.S. regions, compared to 3.2 in urban ones.
How Patients Really Feel About It
Real-world experiences vary, but the pattern is clear: if you’re desperate - if you’ve tried five antidepressants and nothing worked - this can be life-changing.
On Healthgrades, Spravato has a 3.7 out of 5 rating. Sixty-two percent of reviewers mentioned dissociation. Of those, 41% called it ‘manageable.’ Only 21% said it was ‘severe.’ Most said it faded fast. The same survey found that 87% of patients with blood pressure spikes saw them resolve without treatment within 90 minutes.
What people consistently praise is the staff. Ninety-one percent of positive reviews on Drugs.com said, ‘The clinic staff knew exactly what to do.’ That’s the difference between fear and safety. You’re not being watched because you’re risky. You’re being watched because they care enough to make sure you’re okay.
One user wrote: ‘I cried the first time I felt better in years. I didn’t care that I felt like I was floating. I cared that I could breathe again.’

What’s Changing in 2026 - And What’s Not
Things are evolving. In September 2023, the FDA approved a new option: for patients who show stable vitals and mild dissociation after their first few treatments, the monitoring time can be cut from two hours to one. This is based on data from the SUSTAIN-2 trial, which showed that 63% of patients were safe to leave after 60 minutes.
That’s a big deal. It means fewer missed work hours, lower costs, and better access - especially in places where clinics are far away. But it’s not for everyone. Only those who’ve already tolerated the drug well qualify.
Companies are also testing digital tools - apps that let patients self-report dissociation or use smartphone sensors to track heart rate and movement. But don’t expect remote treatment anytime soon. The FDA still says the acute risks of dissociation and blood pressure spikes require in-person oversight. That’s not changing.
And despite the hype around ‘rapid-acting antidepressants,’ Spravato still dominates the market. It generated over $1 billion in global sales in 2022 and is projected to keep growing. Other drugs are coming, but none have matched its effectiveness for treatment-resistant cases.
Who Should Consider Esketamine - And Who Shouldn’t
This isn’t for everyone. You’re a candidate if:
- You have major depression that hasn’t improved after at least two different antidepressants.
- You’re currently experiencing moderate to severe symptoms.
- You’re under the care of a psychiatrist who can coordinate with a certified clinic.
- You don’t have uncontrolled high blood pressure, heart disease, or brain aneurysms.
- You’re willing to commit to the time, cost, and side effects.
You should avoid it if:
- Your blood pressure is over 160/100 at screening.
- You’ve had a heart attack, stroke, or brain bleed in the past year.
- You have a history of psychosis or substance use disorder (unless carefully managed).
- You can’t arrange transportation or time off for two-hour sessions twice a week.
It’s not a miracle cure. But for people who’ve been stuck for years - who’ve lost jobs, relationships, hope - it’s one of the few options that works fast. And that matters.
What Comes After the Spray?
Esketamine doesn’t replace your other antidepressant. You still take your oral medication - usually an SSRI or SNRI. The spray is an accelerator. It gives you a jumpstart. Then your regular meds do the long-term work.
Treatment usually starts with two doses per week for four weeks, then tapers to once a week, then every other week. Most people see improvement within two weeks. The goal is to stabilize mood so you can reduce or eventually stop the spray - while keeping your oral antidepressant going.
Long-term data from the RECOVER study shows no worsening of dissociation or blood pressure with repeated use. That’s reassuring. But it’s still a powerful drug. You’re not on it forever. It’s a bridge - not a destination.






Jacob Cathro
January 19, 2026 AT 00:06thomas wall
January 19, 2026 AT 20:45Paul Barnes
January 20, 2026 AT 23:25pragya mishra
January 21, 2026 AT 19:24Manoj Kumar Billigunta
January 23, 2026 AT 02:33Andy Thompson
January 24, 2026 AT 23:17sagar sanadi
January 26, 2026 AT 14:25kumar kc
January 26, 2026 AT 15:16clifford hoang
January 28, 2026 AT 13:28