When you’re on antibiotics, your gut pays the price. Even if the medicine clears up your infection, it doesn’t discriminate-it kills off the bad bacteria and the good ones. That’s why so many people end up with bloating, cramps, or diarrhea while taking antibiotics. The good news? Probiotics can help. But only if you take them at the right time.
Why Timing Matters More Than You Think
Taking probiotics and antibiotics at the same time is like sending firefighters into a burning building while someone’s still pouring gasoline. The antibiotics will kill the probiotic bacteria before they even have a chance to settle in. Studies show that when people take probiotics within an hour of their antibiotic dose, up to 92% of the beneficial bacteria die off before they can do their job. The solution? Space them out. At least two hours apart. That’s the sweet spot. It gives your body time to process the antibiotic so it doesn’t wipe out the probiotics right away. This isn’t just theory-it’s backed by clinical trials. One 2023 analysis of 19 studies found that people who spaced probiotics at least two hours from antibiotics reduced their risk of antibiotic-associated diarrhea by 64% compared to those who took them together.Which Probiotics Work Best?
Not all probiotics are created equal. Some strains survive better than others, and some don’t even care about antibiotics. Bacterial probiotics like Lactobacillus rhamnosus GG and Bifidobacterium species are sensitive to antibiotics. You need to space these out by two hours. They’re the most common in supplements, so this rule applies to most store-bought products. Yeast-based probiotics like Saccharomyces boulardii CNCM I-745 are different. They’re not bacteria-they’re fungi. Antibiotics don’t touch them. That means you can take this strain at the same time as your antibiotic without losing effectiveness. In fact, studies show it reduces diarrhea risk by 52% when taken daily during antibiotic treatment. If you’re unsure which strain you’re taking, check the label. Look for the full scientific name. If it says “Lactobacillus” or “Bifidobacterium,” space it out. If it says “Saccharomyces boulardii,” you’re good to go together.How Much Should You Take?
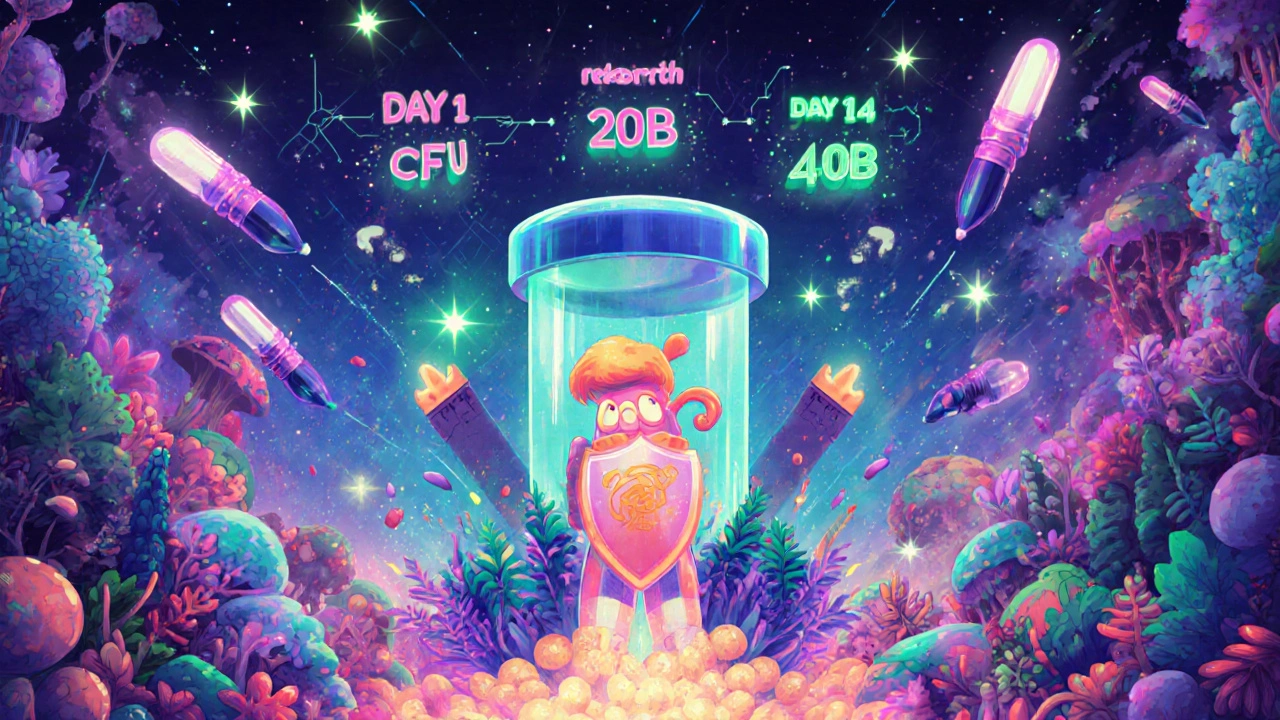
Dose matters. A 5-billion CFU (colony-forming unit) pill won’t cut it if you’re on a two-week course of strong antibiotics. Here’s what the research recommends:- Mild cases (short antibiotic course, no prior gut issues): 5-10 billion CFU per day
- Moderate cases (diarrhea, bloating, or longer course): 10-20 billion CFU per day
- Severe cases (14+ days of antibiotics, history of gut problems): 20-40 billion CFU per day
When to Start-and When to Stop
Don’t wait until you feel sick to start probiotics. The best time is within 48 hours of your first antibiotic dose. Waiting longer cuts the benefit in half. A Cochrane Review showed that starting probiotics after antibiotics ended was 32% less effective at preventing diarrhea than starting while still on the meds. And don’t quit when the antibiotics run out. Your gut needs time to rebuild. Experts recommend continuing probiotics for 7 to 14 days after your last antibiotic pill. One 2024 study tracking gut bacteria recovery found that people who stuck with probiotics for two weeks after antibiotics had 89% of their microbial diversity restored. Those who stopped early? Only 63%.Real-Life Scheduling: Make It Easy
Trying to remember to take something two hours before or after your antibiotic? It’s easy to forget. Here’s how to make it stick. If you take antibiotics twice a day-at 8 a.m. and 8 p.m.-here’s your simple schedule:- 6 a.m.: Probiotic
- 8 a.m.: Antibiotic
- 10 a.m.: Probiotic (if taking twice daily)
- 6 p.m.: Probiotic
- 8 p.m.: Antibiotic
- 10 p.m.: Probiotic (if taking twice daily)
What Not to Do
The biggest mistake? Taking probiotics at the same time as antibiotics. It doesn’t just reduce effectiveness-it defeats the whole purpose. In vitro tests show up to 92% of the probiotic bacteria die when exposed to antibiotics without spacing. Another common error: stopping probiotics too soon. People think, “I’m done with antibiotics, I’m fine now.” But your gut is still recovering. Skipping those extra 7-14 days means your microbiome never fully bounces back. Also, don’t assume “more strains = better.” A 2023 meta-analysis found no significant difference between single-strain and multi-strain probiotics for preventing antibiotic diarrhea. What matters is the strain type, dose, and timing-not the number of ingredients on the label.What About Food?
Probiotics don’t need to be taken on an empty stomach. In fact, some research suggests taking them with a small meal-especially one with healthy fats-can help them survive stomach acid better. Avoid taking them with hot drinks or alcohol, which can kill the live cultures. Fermented foods like yogurt, kefir, sauerkraut, and kimchi contain natural probiotics. But they’re not strong enough to replace a supplement during antibiotic treatment. Think of them as a nice bonus, not your main defense.What’s Changing in 2025?
New research is showing that probiotics aren’t a one-size-fits-all fix. Some strains might even slow down gut recovery in certain people. Stanford University is now running trials to match probiotics to individual microbiome profiles after antibiotics. Companies are also developing time-release capsules and acid-resistant coatings that protect probiotics from antibiotics. These might one day eliminate the need for strict spacing. But as of late 2024, none are approved as standard care. For now, the 2-hour rule still stands. It’s backed by 27 of the 31 major medical institutions’ antibiotic stewardship programs. And with 30% of antibiotic users developing digestive issues, skipping this step isn’t worth the risk.Can I take probiotics and antibiotics at the same time?
Only if the probiotic is Saccharomyces boulardii, a yeast strain unaffected by antibiotics. All bacterial probiotics-like Lactobacillus and Bifidobacterium-must be spaced at least two hours apart from antibiotics. Taking them together kills up to 92% of the beneficial bacteria before they can work.
How long should I take probiotics after antibiotics?
Continue for 7 to 14 days after your last antibiotic dose. Studies show this is when your gut microbiome begins to recover most rapidly. Stopping too soon means you miss the window for rebuilding healthy bacteria, and your risk of long-term digestive issues stays higher.
What CFU count should I look for in a probiotic?
For most people on antibiotics, aim for 10-20 billion CFUs per day. If you’re on a long course (over 14 days) or have a history of gut problems, go with 20-40 billion CFUs. Lower doses (5-10 billion) are fine for short courses and mild symptoms, but won’t be enough for significant protection.
Do I need a multi-strain probiotic?
No. Research shows multi-strain products offer no real advantage over single-strain ones for preventing antibiotic diarrhea. What matters more is choosing the right strain-Lactobacillus rhamnosus GG or Saccharomyces boulardii-and taking the right dose at the right time.
Can I get enough probiotics from yogurt or fermented foods?
Fermented foods like yogurt and kimchi contain probiotics, but not in high enough doses to reliably prevent antibiotic-associated diarrhea. They’re great for general gut health, but during antibiotic treatment, you need the concentrated, clinically tested doses found in supplements.
What if I forget to space my probiotic and antibiotic?
If you accidentally take them together, don’t panic. Just wait at least two hours before taking your next probiotic dose. Don’t double up to make up for it. Consistency over time matters more than perfect timing on every single dose. Missing one dose won’t ruin your results-skipping multiple doses will.







Nathan Hsu
November 13, 2025 AT 01:17Wow, this is gold-seriously, someone should print this out and tape it to every pharmacy counter in India. I’ve seen my uncle take antibiotics and then immediately chug yogurt like it’s a magic potion… and then he wonders why he’s stuck to the toilet for a week. Two-hour rule? Yes. Saccharomyces boulardii? Yes. Dose matters? YES. Stop treating your gut like a suggestion box.
Ashley Durance
November 13, 2025 AT 06:26Let’s be real-most people don’t even know what CFU means. And yet, they buy the most expensive probiotic on the shelf because it has ‘100 billion’ printed in neon letters. The 2023 meta-analysis you cited? It’s buried in the supplemental data of a journal no one reads. And you’re acting like spacing doses by two hours is some revolutionary breakthrough. It’s basic pharmacology. Also, ‘fermented foods aren’t strong enough’? That’s not even scientifically nuanced-it’s lazy.
Scott Saleska
November 14, 2025 AT 09:53I appreciate the breakdown, but I have to push back a little-your 2-hour rule might be the minimum, but for broad-spectrum antibiotics like clindamycin, I’ve seen studies where 4–6 hours makes a huge difference in bacterial survival. I’m not a doctor, but I’ve read the papers. Also, if you’re taking probiotics twice a day, why not space them 4 hours apart from the antibiotic? That gives the bacteria a longer window to colonize. And don’t forget-some probiotics are spore-forming now, like Bacillus coagulans. They’re even tougher than Saccharomyces. Maybe we need to update the guidelines?
Ryan Anderson
November 14, 2025 AT 20:57This is the kind of post that saves people from months of bloating and regret 🙌 I’ve been on antibiotics three times in the last year, and I wish I’d read this before my first round. I took probiotics with my meds… and spent a week in sweatpants. Now I’m doing 20 billion CFU of L. rhamnosus GG at 6 a.m. and 6 p.m., antibiotic at 8 a.m. and 8 p.m. - it’s like a little ritual now. My gut is actually happy. Thank you for the schedule-it’s the only thing I’ve actually followed.
Eleanora Keene
November 15, 2025 AT 10:08Okay, I’m not a scientist, but I’ve been helping my mom through her antibiotics and I just wanted to say thank you for making this so clear. I printed this out and put it next to her pill organizer. She’s 72, doesn’t use her phone much, but she reads this every morning. We’re on day 10, and she hasn’t had a single episode of diarrhea. You’re right-starting within 48 hours made all the difference. And we’re continuing for two more weeks. You’ve changed our routine for the better.
Joe Goodrow
November 16, 2025 AT 15:00Probiotics? Sounds like liberal pseudoscience to me. Back in my day, we just drank buttermilk and toughed it out. Now everyone’s got a pill for everything. You’re telling me we need to time this like a NASA launch? That’s not medicine-that’s overcomplicating. Antibiotics work. Your gut will heal. Stop buying into the supplement industrial complex.
Kevin Wagner
November 17, 2025 AT 22:26Y’all are overthinking this. This isn’t rocket science-it’s gut science. And if you’re not taking at least 20 billion CFUs, you’re wasting your money. I’m on cipro right now, and I’m taking Saccharomyces boulardii with my antibiotic AND a 40-billion dose of L. rhamnosus two hours later. My gut’s been smoother than a baby’s butt. Don’t be cheap with your microbiome. Your colon will thank you. And yes, I’m a believer. This isn’t woo-woo-it’s biology with receipts.
gent wood
November 19, 2025 AT 13:51