Every year, over 108,000 people in the U.S. die from drug overdoses. Most of those deaths involve synthetic opioids like fentanyl-but many started with a prescription for pain. The truth is, opioid safety isn’t just about stopping bad behavior. It’s about changing how we think about pain, prescribing, and care. If you’re a patient managing chronic pain, or a clinician trying to do right by your patients, the rules have changed. And they’re not going back.
Why the Rules Changed
Ten years ago, opioids were seen as a go-to solution for almost any kind of pain. But by 2020, it was clear something had gone wrong. Too many people got hooked. Too many overdoses happened. Too many families lost someone to a pill that was supposed to help. In 2025, the CDC, FDA, and CMS rolled out the most significant updates to opioid prescribing guidelines in over a decade. These weren’t just tweaks. They were a full reset. The goal? Keep people out of the hospital, out of addiction, and alive-without leaving others in unbearable pain. The data drove the change. Studies showed that once a patient hits 50 morphine milligram equivalents (MME) per day, their risk of overdose jumps nearly threefold. At 90 MME, the risk becomes extreme. And for acute pain-like after a dental procedure or a sprained ankle-just one extra day of opioids increases the chance of long-term use by 20%.What the 2025 Guidelines Actually Say
The new rules are specific. No guessing. No exceptions unless they’re clearly justified.- For acute pain, the default is a three-day supply. Seven days is only allowed if your doctor documents why-like after major surgery or severe trauma.
- Doses above 50 MME per day require a full risk assessment and regular follow-ups. Anything above 90 MME should be avoided unless you’re in palliative care or have cancer.
- Every prescription for opioids must now be checked against your state’s Prescription Drug Monitoring Program (PDMP). This isn’t optional. It’s built into the electronic health record system.
- Pharmacies can’t fill an initial opioid prescription for more than three days for acute pain. That’s a hard stop. No exceptions.
Who’s Affected-and How
This isn’t just about new patients. It’s also about the 1.5 million Americans who’ve been on long-term opioids for years. Some people are doing fine. They’ve been on stable doses for a decade, with no signs of misuse. But now, their doctors are being pressured to taper them down. And that’s where things get dangerous. The FDA made this clear in their 2025 labeling update: Don’t rush the taper. Abruptly stopping opioids can trigger severe withdrawal, uncontrolled pain, and even suicide. A 2024 study found a 23% spike in suicide attempts among patients whose doses were cut too fast. That’s why the VA and CDC now recommend a slow, patient-led approach. If you’ve been on opioids for years, your doctor should work with you-not against you. Tapering should be done in small steps, with non-opioid options in place first.What Works Better Than Opioids
The biggest shift isn’t in the rules. It’s in the tools. You don’t need opioids for most pain. Here’s what actually works:- NSAIDs like ibuprofen or naproxen-just as effective for joint and muscle pain, with far lower risk.
- Acetaminophen combinations-safe when used correctly, and often combined with NSAIDs for better results.
- Physical therapy-studies show it reduces opioid use by 40% in patients with back pain.
- Cognitive behavioral therapy (CBT)-helps rewire how your brain processes pain signals. Proven to reduce pain intensity and opioid dependence.
- CBD-based products-growing fast. Some patients report significant relief without the high or addiction risk.

The Real Challenge: Access and Equity
Here’s the uncomfortable truth: these guidelines work best when you have resources. A patient in rural West Virginia might not have a physical therapist within 50 miles. A single mom working two jobs can’t take time off for weekly CBT sessions. A veteran with PTSD and chronic pain might need a team, not just a prescription. The system isn’t ready. There’s a shortage of 12,500 pain specialists nationwide. Rural counties are especially underserved-68% don’t have a dedicated pain clinic. And when patients can’t get alternatives, they suffer. The U.S. Pain Foundation found that 7-10% of long-term opioid users were abruptly cut off in 2024-2025. Many ended up in emergency rooms because their pain returned with no safe way to manage it. The goal isn’t to punish. It’s to protect. But protection only works if the alternatives are actually available.What Patients Should Do
If you’re on opioids for pain:- Ask your doctor: “Is this the lowest effective dose?”
- Ask: “What non-opioid options have we tried?”
- Ask: “Can we set up a plan to slowly reduce this, if it’s safe?”
- Don’t hide other medications or substances. Alcohol, benzodiazepines, and sleep aids mix dangerously with opioids.
- Know your PDMP. Most states let you check your own prescription history online. It’s your right.
- Take only what you need. Don’t save them. Don’t share them.
- Dispose of unused pills. Many pharmacies have drop boxes.
- Set a clear end date. If you’re still taking them after 7 days, talk to your doctor.
What Clinicians Need to Know
Doctors aren’t the enemy here. They’re caught in the middle. The paperwork has doubled. A note for a patient on 50+ MME now takes 27% longer to write. Electronic systems aren’t always smooth. Some practices spend 2-3 extra hours a week just on opioid documentation. But the tools are there:- Use the Opioid Risk Tool (ORT) or SOAPP to screen for addiction risk.
- Check PDMP before every opioid prescription. It cuts overlapping prescriptions by 37%.
- Use the VA’s OSI Toolkit if you manage complex cases-it integrates mental health, substance use, and pain history.
- Partner with physical therapists, psychologists, and pharmacists. Team-based care reduces opioid use without sacrificing pain control.
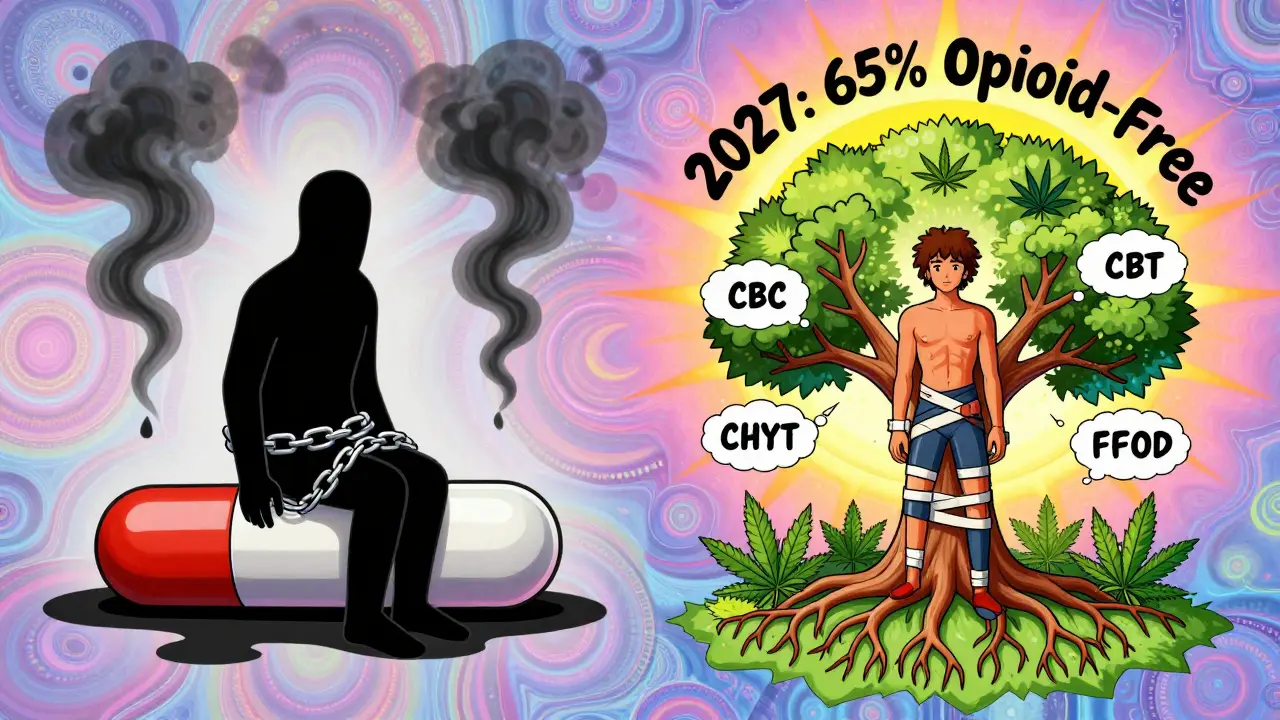
The Future Is Non-Opioid
By 2027, 65% of acute pain cases will be managed without opioids. That’s up from 48% in 2025. Why? Because the science is clear. NSAIDs, physical therapy, nerve blocks, and psychological support work. They’re safer. They’re cheaper. And they don’t kill. The NIH is pouring $125 million into new non-addictive pain treatments. Companies are developing targeted nerve blockers, wearable pain devices, and AI-driven pain management apps. The old model-reach for the pill first-is ending. The new model-build a plan, use the least risky tool first-is here. It’s not perfect. It’s not easy. But it’s working.Final Thought
Pain is real. So is addiction. The goal isn’t to choose one over the other. It’s to treat pain without creating a new crisis. The 2025 guidelines aren’t about restriction. They’re about responsibility. About knowing when a pill helps-and when it harms. About giving people real tools, not just temporary relief. The next five years will define whether we finally get this right. And it starts with one question: What’s the next step after the opioid?Can I still get opioids for chronic pain?
Yes-if your doctor determines it’s necessary and safe. The guidelines don’t ban opioids for chronic pain. But they require strict documentation, regular monitoring, and a clear plan for non-opioid alternatives. Doses above 90 MME per day are strongly discouraged unless you have cancer, are in palliative care, or have other exceptional circumstances.
What if my pain gets worse after a three-day supply runs out?
That’s why the three-day limit isn’t a hard cutoff-it’s a starting point. If your pain continues, you should return to your doctor. They’ll reassess your condition and explore other options: physical therapy, nerve blocks, anti-inflammatories, or a longer-term non-opioid plan. Never self-medicate with leftover pills or someone else’s medication.
Are the new rules the same in every state?
No. While federal guidelines (CDC, CMS, FDA) set the floor, 38 states have their own laws on acute pain prescriptions-some limit it to 3 days, others allow 5 or 7. Pharmacies must follow the stricter rule. Always check your state’s current limits, especially if you travel or get prescriptions from out-of-state providers.
How do I know if I’m at risk for opioid addiction?
Doctors use tools like the Opioid Risk Tool (ORT) or SOAPP. Factors include personal or family history of substance use, mental health conditions like depression or PTSD, and previous opioid misuse. If you’ve ever struggled with alcohol, smoking, or drugs, tell your doctor. It’s not judgment-it’s safety.
Can I get help if I’m already dependent on opioids?
Absolutely. Medication-assisted treatment (MAT) with buprenorphine or naltrexone is proven to reduce overdose risk and help people regain control. Many clinics now offer integrated pain and addiction care. If you’re worried about dependence, talk to your doctor or call the SAMHSA National Helpline at 1-800-662-HELP (4357). You’re not alone.
What should I do with unused opioid pills?
Don’t flush them or throw them in the trash. Many pharmacies have drug take-back bins. If none are nearby, mix the pills with coffee grounds or cat litter, seal them in a container, and throw them in the household trash. This prevents accidental ingestion or misuse.
Why are dentists and surgeons prescribing less now?
Because the data shows they didn’t need to prescribe so much in the first place. A 2025 study found dental opioid prescriptions dropped 63% after the three-day limit took effect. Most patients only needed NSAIDs. Surgeons are now using long-acting local anesthetics and nerve blocks instead of opioids for post-op pain. The change is working.





Molly Silvernale
January 8, 2026 AT 08:44So we’re saying pain is a philosophical problem now? Not a biological one? I mean… if you’ve got a spine that’s decided to turn into a broken violin, and the only thing that quiets the screaming is a little white pill-why are we treating that like a moral failure? The system wants to fix pain with spreadsheets and therapy sessions, but the body doesn’t care about your policy memo. It just wants relief. And sometimes? Relief looks like a 30mg oxycodone. Not a yoga mat.
christy lianto
January 8, 2026 AT 20:31Y’ALL. I’ve been on 70 MME for 8 years. They tried to taper me last year-Rushed it. I lost my job. I lost my kids’ trust. I lost sleep. I almost lost myself. Then I found a pain clinic that actually listened. They added PT, CBT, and a CBD patch. Not a magic bullet. But a lifeline. Don’t cut people off. Build bridges. And for god’s sake-stop acting like opioids are the devil when the system abandoned us first.
Ken Porter
January 10, 2026 AT 09:53Another liberal overreach. The government thinks it knows better than my doctor. I’ve got a herniated disc. I need my meds. If you can’t handle responsibility, don’t prescribe. But don’t take my pain relief away because you’re scared of a few bad apples.
swati Thounaojam
January 10, 2026 AT 18:34in india we dont even get ibuprofen easy… how u expect us to get PT or cbt? this rules good for usa but not for world
Annette Robinson
January 12, 2026 AT 10:22I’ve worked with chronic pain patients for 15 years. The ones who thrive? They’re the ones who get a team-not just a script. A PT who knows their body. A therapist who gets their anxiety. A pharmacist who checks in. It’s not about taking away opioids. It’s about giving people more tools. And that takes time, money, and compassion. We can do better. We just have to choose to.
Luke Crump
January 13, 2026 AT 14:27Oh wow. The 2025 guidelines. The great opioid purge. The day the medical establishment decided pain was a sin. Next they’ll ban crying. And then breathing. Because *gasp* it might lead to suffering. I mean, I get it-people die. But so do people who are left to scream into the void because their doctor’s too afraid to write a prescription. This isn’t safety. It’s control dressed up in data.
Dave Old-Wolf
January 13, 2026 AT 19:24I’m a veteran. Had back pain since Iraq. Took opioids for 12 years. Got tapered too fast. Ended up in the ER with panic attacks and muscle spasms. Then I found a VA program that did CBT + acupuncture + low-dose naltrexone. Took 6 months. But I’m off opioids now-and I can play with my grandkids without feeling like my spine’s on fire. It’s not easy. But it’s possible.
Donny Airlangga
January 13, 2026 AT 20:53Just read this whole thing. Honestly? It’s the most balanced thing I’ve seen on this topic. The part about rural access hit me hard. My aunt lives in Montana. No PT within 100 miles. Her doctor just kept giving her pills because he had no other options. This isn’t about being tough. It’s about being fair. We need to fund the alternatives. Not just ban the pills.
Kristina Felixita
January 14, 2026 AT 20:21OMG I just found out my state lets you check your PDMP online?? I’ve been on a script for 3 years and never checked!! Just looked it up… and holy moly, I’ve had 4 different doctors prescribe me this in the last year!! No wonder I felt foggy!! I’m calling my doc tomorrow-thank you for this post!! 🙏❤️
Joanna Brancewicz
January 16, 2026 AT 06:42Non-opioid modalities: NSAIDs, CBT, PT. All evidence-based. But the real barrier? Reimbursement. Medicare pays $120 for an opioid script. $45 for a 45-min PT session. $0 for CBT if the therapist isn’t in-network. So of course doctors reach for the pill. It’s not malice. It’s economics.
Evan Smith
January 16, 2026 AT 18:20So… we’re gonna replace opioids with yoga and apps? Cool. Next time I break my ankle, I’ll just meditate and wait for my AI pain coach to send me a motivational meme. 😏 Meanwhile, my doctor’s got 12 patients waiting and 5 minutes to make a decision. Sometimes the pill is the only sane choice. Let’s fix the system. Not just the script.