Medication-Induced Hair Loss Calculator
Estimate your hair loss timeline
This tool helps you understand whether your hair loss might be medication-induced based on timing and medication type.
Key Takeaways
- Medication‑induced hair loss, also called drug‑induced alopecia, usually appears 2‑4 months after starting a new drug.
- Two main mechanisms drive the loss: telogen effluvium (resting‑phase shedding) and anagen effluvium (rapid growth‑phase loss).
- Common offenders include chemotherapy, methotrexate, oral retinoids, and several antidepressants.
- Stopping the culprit drug is the most effective step; most cases improve within 6‑9 months.
- Adjunct treatments-minoxidil, scalp‑cooling, low‑level laser therapy, and targeted supplements-boost regrowth in stubborn cases.
What is medication‑induced hair loss?
Medication‑Induced Hair Loss is a form of drug‑induced alopecia where pharmaceutical agents trigger abnormal shedding or thinning of scalp hair. It can be reversible or, in rare cases, permanent, depending on the drug class and individual susceptibility.
The condition was first described in dermatology journals in the 1950s as new chemotherapy agents entered clinical use. Today, clinicians recognize it as a side effect affecting roughly 1‑10 % of patients who take high‑risk medications.
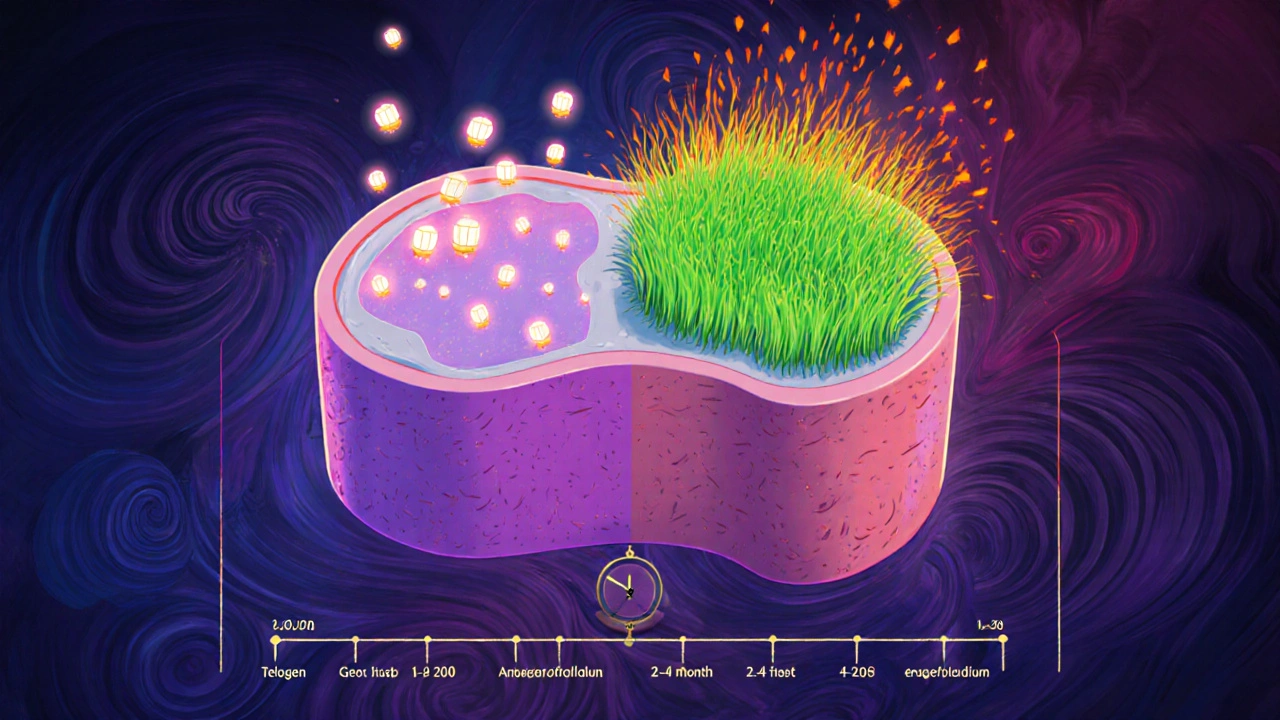
How the drugs mess with your hair cycle
Hair grows in a predictable three‑phase cycle: anagen (growth), catagen (transition), and telogen (rest). Two drug‑related pathways break this rhythm.
Telogen Effluvium forces follicles into the telogen phase prematurely. Shedding typically begins 2‑4 months after the offending drug starts, peaks around 3‑5 months, and often resolves on its own within 6‑9 months once the medication is stopped.
Anagen Effluvium is a rapid loss that occurs while hair is still in the active anagen phase. Chemotherapy drugs are the classic culprits, causing noticeable thinning within 7‑14 days of the first infusion.
Medications most likely to cause hair loss
- Chemotherapy agents - up to 65 % of patients experience anagen effluvium.
- Methotrexate - 1‑3 % of rheumatoid‑arthritis users report telogen‑type shedding.
- Leflunomide - about 10 % incidence in the same patient group.
- Oral retinoids (isotretinoin, acitretin) - roughly 18 % of dermatology patients notice thinning.
- Selective serotonin reuptake inhibitors (SSRIs) - 5‑7 % of antidepressant users develop telogen effluvium.
- Beta‑blockers, antihypertensives, and antiepileptics - lower‑frequency reports but still worth checking.
When you start a new prescription, ask your pharmacist or doctor if hair loss is listed as a side effect. A quick medication‑history review can save months of anxiety.
Spotting the problem early
The “7‑month rule” is a simple diagnostic aid: any drug started within the last seven months of unexplained shedding should be flagged as a potential cause. Look for diffuse thinning rather than patchy bald spots-that pattern points to a systemic trigger.
Typical timelines:
| Mechanism | Typical Onset | Resolution (if drug stopped) |
|---|---|---|
| Telogen effluvium | 2‑4 months | 6‑9 months |
| Anagen effluvium | 7‑14 days | 3‑6 weeks after chemo ends |
First line: stop or switch the offending drug
If the medication isn’t essential, your clinician will typically taper or replace it. Studies from the Mayo Clinic show that 85 % of telogen‑effluvium cases resolve spontaneously within six months after discontinuation.
When stopping isn’t an option (e.g., life‑saving chemotherapy), we move to supportive therapies.
Topical and oral treatments that help
- Minoxidil - 5 % solution applied twice daily improves hair density in 40‑50 % of users after six months. Expect an initial shedding phase (weeks 2‑8).
- Finasteride - 60‑65 % efficacy for androgen‑linked drug‑triggered loss; oral dose 1 mg daily.
- Dutasteride - slightly higher response (70‑75 %) but more systemic side effects.
- Folic acid (1 mg daily) can cut methotrexate‑related shedding by ~25 %.
- Biotin, zinc, iron - daily supplementation supports overall follicle health, especially if labs show a deficiency.
Procedural options for stubborn cases
When topical agents fall short, consider:
- Scalp cooling (e.g., DigniCap) - applied 15 min before, during, and 30 min after chemotherapy; retains 50‑65 % of hair in breast‑cancer protocols.
- Low‑level laser therapy (LLLT) - devices like iRestore Elite require daily 20‑30 min sessions for 26 weeks to achieve statistically significant density gains.
- Exosome therapy - early‑stage trials show a 30 % increase in density at six months, though still experimental.
Practical checklist for patients
- Write down every medication taken in the past year, including over‑the‑counter supplements.
- Match the start date against the 7‑month rule.
- Discuss with your prescriber whether a switch or dose reduction is feasible.
- If you must stay on the drug, begin minoxidil (or finasteride for men) after a three‑month observation period.
- Schedule a blood panel for ferritin, zinc, and vitamin D; correct deficiencies.
- Consider adjuncts like scalp cooling or LLLT if you’re undergoing chemotherapy.
- Track progress with monthly photos; most regrowth appears after 4‑6 months of consistent treatment.
When to seek professional help
If shedding exceeds 100 hairs per day, persists beyond nine months after drug cessation, or is accompanied by scalp pain, scalp infection, or sudden patchy loss, see a dermatologist. Early referral improves the chance of identifying an overlapping condition such as alopecia areata.
Future outlook
Genetic testing is on the horizon: the Mayo Clinic identified 17 single‑nucleotide polymorphisms linked to higher risk of drug‑induced alopecia, promising 82 % predictive accuracy. In the next few years, doctors may run a quick cheek‑swab before prescribing high‑risk meds, tailoring therapy to keep your hair safe.

Key takeaway for today’s readers
If you’re dealing with medication induced hair loss, the first step is a thorough med‑review and, whenever possible, stopping the offending drug. Most cases improve on their own, and a toolbox of proven treatments-minoxidil, finasteride, scalp cooling, and laser therapy-can accelerate regrowth and restore confidence.
How long does medication‑induced hair loss usually last?
Most telogen‑effluvium cases resolve within 6‑9 months after the drug is stopped. Anagen effluvium from chemotherapy typically sees regrowth start 3‑6 weeks after the treatment ends, with full density returning in 3‑6 months.
Can I prevent hair loss if I need to stay on the medication?
While the safest approach is to switch drugs, adjuncts like low‑dose minoxidil, folic acid (for methotrexate), and scalp‑cooling during chemotherapy can significantly reduce the severity of loss.
Is hair loss from antidepressants permanent?
Usually not. Antidepressant‑related telogen effluvium often reverses once the drug is tapered or switched. In rare cases, a short course of minoxidil can speed up regrowth.
Should I take supplements without a doctor’s order?
It’s best to get a baseline blood test. If you’re low in iron, zinc, or biotin, targeted supplementation for at least six months can improve outcomes. Unchecked high doses may cause other issues.
Does scalp cooling hurt?
Patients report a moderate discomfort level (about 7/10) during the 90‑minute cooling session, but many consider the trade‑off worth it for the hair they keep.



Jennie Smith
October 25, 2025 AT 15:46Wow, that checklist feels like a bright roadmap for anyone battling drug‑induced hair loss!
Greg Galivan
October 25, 2025 AT 17:10The article kinda oversimplifies telogen effluvium – it’s not just a 2‑4 month thing. Docs need to check labs before tossing minoxidil at patients. Also, the “7‑month rule” sounds like a guess, not a science.
Anurag Ranjan
October 25, 2025 AT 18:33When you start a new med write down the exact start date it helps match the 7‑month rule. If you notice shedding early ask your doc about a possible switch or dose tweak.
James Doyle
October 25, 2025 AT 19:56The mechanistic underpinnings of drug‑induced alopecia are far more intricate than the superficial overview suggests.
The pharmacodynamic interactions can precipitate a cascade of follicular apoptosis, particularly when cytotoxic agents intersect with the anagen phase.
Meanwhile, telogen effluvium operates via a dysregulation of the hair cycle’s homeostatic checkpoints, often mediated by inflammatory cytokines.
Clinicians must therefore adopt a multidimensional diagnostic algorithm that incorporates temporal drug exposure, laboratory indices, and scalp trichoscopy.
The so‑called '7‑month rule' is a heuristic at best and should not supplant a personalized risk assessment.
In practice, a thorough med‑review coupled with a withdrawal or substitution strategy yields the highest probability of regrowth.
Adjunctive therapeutics such as minoxidil function by prolonging the anagen phase through vasodilatory and proliferative mechanisms.
Finasteride, by inhibiting 5‑alpha‑reductase, attenuates dihydrotestosterone‑driven miniaturization, a process not exclusive to androgenic alopecia.
For patients undergoing chemotherapy, the integration of scalp‑cooling devices can mitigate follicular toxicity by reducing local thermoregulation.
Low‑level laser therapy, despite its modest evidence base, is postulated to enhance mitochondrial activity within dermal papilla cells.
Emerging modalities like exosome infusion aim to deliver extracellular vesicles rich in growth factors to rejuvenate the follicular niche.
Nevertheless, insurance coverage for such cutting‑edge interventions remains sporadic and often contingent upon documented treatment failure.
From a psychosocial perspective, the abrupt loss of hair can precipitate significant emotional distress, underscoring the need for holistic patient counseling.
It is also prudent to evaluate nutritional status, as deficiencies in iron, zinc, and biotin can exacerbate shedding trajectories.
Future genomic screening may soon enable preemptive identification of polymorphisms linked to heightened susceptibility.
Until such precision tools become mainstream, the cornerstone of management remains vigilant monitoring, judicious drug selection, and evidence‑based supportive care.
Edward Brown
October 25, 2025 AT 21:20One can't help but wonder if the pharmaceutical giants are quietly engineering these side effects to churn a market for pricey hair‑restoration products. The data on genetic predictors feels like a breadcrumb left for us to follow not a clear road. While doctors cite 'clinical guidelines' those are often drafted behind closed doors where lobbyists roam. If we keep accepting minoxidil as a panacea we may never see the hidden agenda. Trusting the system demands more than just reading a checklist.
ALBERT HENDERSHOT JR.
October 25, 2025 AT 22:43It's commendable that you're taking a systematic approach to this challenge; documenting every medication and aligning it with the 7‑month rule lays a solid foundation. Pairing that diligence with a structured regimen of minoxidil and, where appropriate, finasteride can significantly boost regrowth outcomes. Remember to re‑evaluate blood work periodically to address any micronutrient gaps that might impede recovery :)
Suzanne Carawan
October 26, 2025 AT 00:06Oh sure, just pop a bottle of minoxidil and all that hair will magically sprout back. As if doctors haven't been saying that for decades.
Kala Rani
October 26, 2025 AT 01:30Actually the whole idea of 'just wait' is a myth. You need active intervention not passive hope