It’s easy to assume that if you break out in hives after eating or taking something, it’s an allergy. But not all reactions are created equal. A rash after taking amoxicillin might be a true drug allergy. A tingling tongue after eating peanuts could be a life-threatening food allergy. Yet many people mix them up - and that can be dangerous.
How Your Body Reacts Differently
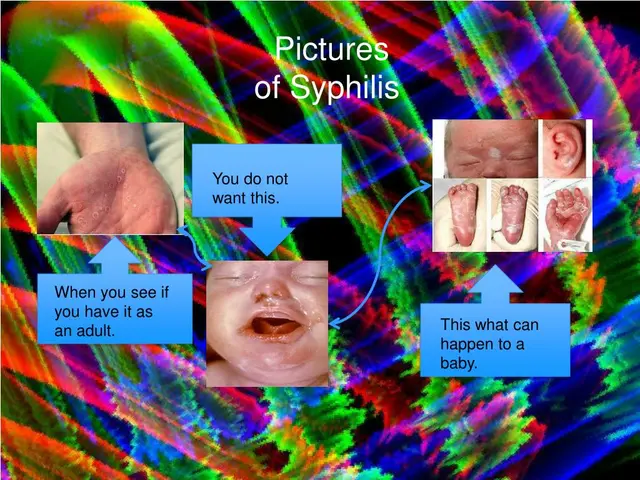
Food allergies and medication allergies both involve your immune system overreacting to something harmless. But the way they trigger that response is different. Most food allergies - about 90% of them - are IgE-mediated. That means your body produces a specific antibody called immunoglobulin E when it sees the allergen. This kicks off a rapid chain reaction: histamine floods your system, blood vessels leak fluid, muscles tighten. That’s why symptoms like swelling, hives, vomiting, or trouble breathing show up within minutes - often under 20 minutes. Medication allergies can also be IgE-mediated, but they’re more complex. About 80% of immediate drug reactions follow the same IgE path. But the other 20%? Those are T-cell driven and slow. You might take a pill on Monday and not see a rash until Friday. Or develop a fever and swollen lymph nodes two weeks later. These delayed reactions include conditions like DRESS syndrome or Stevens-Johnson syndrome - rare, serious, and often mistaken for infections.What the Symptoms Look Like
When you have a food allergy, your body tends to react in predictable places. Oral allergy syndrome - itching or swelling of the lips, tongue, or throat - happens in 70% of cases. Gastrointestinal symptoms like vomiting or diarrhea are common, especially in kids. Hives appear in nearly 9 out of 10 reactions. Anaphylaxis, the most dangerous reaction, can strike within minutes and needs epinephrine right away. Medication allergies often show up as skin rashes. A flat, red, itchy rash (maculopapular) is the most common sign, especially with antibiotics like amoxicillin. Hives can happen too, but they’re less frequent than with food. Respiratory symptoms like wheezing or throat tightness occur in about 40% of immediate drug reactions. But here’s the key difference: food allergies rarely cause fever or joint pain. Medication allergies? Those are common in delayed reactions. If you get a fever, swollen glands, or muscle aches days after taking a drug, it’s more likely a drug reaction than a food allergy.Timing Is Everything
This is one of the clearest ways to tell them apart. Food allergy symptoms almost always show up within two hours - usually within 20 minutes. If you eat shrimp and your lips swell 30 minutes later? That’s a classic food allergy. If you take a pill and feel fine for 48 hours, then break out in a rash? That’s likely a medication reaction. Medication allergies have two distinct windows. Immediate reactions happen within an hour - think hives or anaphylaxis after an IV antibiotic. Delayed reactions? They can take days or even weeks. A rash from amoxicillin during a viral infection is often mislabeled as an allergy. But if you had the same rash after every dose of amoxicillin over three different illnesses? That’s more likely a true allergy.
Diagnosis Isn’t Just About Symptoms
Many people think if they had a reaction once, they’re allergic forever. That’s not true - especially with medications. Up to 90% of people who say they’re allergic to penicillin aren’t when tested. Doctors use skin tests and blood tests for food allergies. Skin prick tests are 90% accurate for IgE-mediated food allergies. If the test is negative, you might still need an oral food challenge - eating the food under supervision - to be sure. That’s the gold standard. For medications, testing is trickier. Penicillin skin testing, followed by an oral challenge, is 99% accurate at ruling out a true allergy. But for most other drugs - like NSAIDs, sulfa drugs, or chemotherapy - there’s no reliable test. Doctors rely on detailed history and, sometimes, a controlled drug provocation test. This isn’t done lightly. It’s risky. But it’s the only way to confirm whether a reaction was truly allergic or just a side effect.Why Getting It Right Matters
Mistaking a food intolerance for an allergy can be deadly. People with true peanut allergies who dismiss early symptoms as indigestion risk anaphylaxis. One study found 22% of food allergy patients didn’t realize their symptoms were serious until they almost died. On the flip side, mislabeling a medication reaction as an allergy has huge consequences. If you’re told you’re allergic to penicillin and you’re not, you’ll likely get a broader-spectrum antibiotic. Those drugs are 30% more expensive and increase your risk of C. diff infection by 25%. They also contribute to antibiotic resistance. In hospitals, unnecessary penicillin avoidance leads to longer stays and higher costs. One case from a 2022 journal involved a woman who avoided all NSAIDs for 10 years because she thought she was allergic to aspirin. Turns out, her rash came from the lactose filler in the pill - not the aspirin itself. She could have safely taken any NSAID all along.What You Should Do
If you’ve had a reaction, write it down. Not just what you ate or took - but when it happened, how long after, what the symptoms were, and how long they lasted. Did you feel fine the next time you ate that food? Did you react to every dose of that drug? Did you have a fever? Swollen glands? These details matter. For food allergies, keep a food-symptom diary. Note the exact food, how it was prepared, and the time between eating and symptoms. Even 5-minute precision helps. For medications, record the brand and generic name, dosage, route (pill, shot, IV), and whether you’ve had the same drug before. Talk to an allergist. Don’t assume. If you think you’re allergic to penicillin, get tested. If your child broke out in hives after peanut butter, don’t just avoid peanuts - get a proper diagnosis. Most children outgrow milk and egg allergies by age 5. But without testing, you’ll never know if it’s safe to reintroduce them.





mark shortus
December 18, 2025 AT 06:28THIS IS THE MOST IMPORTANT THING I’VE READ ALL YEAR. I THOUGHT I WAS ALLERGIC TO PENICILLIN FOR 15 YEARS BECAUSE I GOT A RASH ONCE WHILE SICK. TURNED OUT I HAD MONONUCLEOSIS. I COULD’VE BEEN TAKING THE BEST ANTIBIOTIC FOR MY SINUS INFECTIONS THIS WHOLE TIME. I’M CRYING. I’M SO ANGRY. I’M SO RELIEVED. I’M GOING TO CALL MY ALLERGIST TOMORROW. SOMEONE PLEASE TELL EVERYONE THIS. I’M SHAKING.
IF YOU’RE READING THIS AND YOU THINK YOU’RE ALLERGIC TO SOMETHING - GET TESTED. DON’T JUST LIVE IN FEAR. YOU MIGHT BE DENYING YOURSELF LIFE-CHANGING MEDS. I’M NOT KIDDING. THIS ISN’T DRAMA. THIS IS SURVIVAL.
Elaine Douglass
December 18, 2025 AT 17:12thank you for writing this i had no idea most people who think theyre allergic to penicillin actually aint
my mom always said dont take penicillin but now im gonna ask my doctor about testing
so much less scary than avoiding all antibiotics forever
Emily P
December 20, 2025 AT 05:58Interesting that CRD can distinguish between peanut allergy and birch pollen cross-reactivity. I’ve had oral itching with raw apples and almonds my whole life but never with roasted ones. Never realized it might be oral allergy syndrome. I assumed it was just ‘sensitive mouth.’ Wonder if I’m actually safe with peanut butter if it’s roasted and processed. Should I get tested or just keep avoiding raw nuts? I don’t want to risk it, but I also don’t want to live without peanut butter.
Vicki Belcher
December 20, 2025 AT 19:57OMG THIS IS SO IMPORTANT 🥹🙌
My cousin almost died because she thought her hives after penicillin were 'just a rash' and didn't go to the ER. She’s fine now but terrified to take ANY medicine. I’m sending this to her right now. Please, if you’ve ever had a reaction - don’t assume. Get tested. Your life might literally depend on it. 💙💊
Also - if you’re allergic to peanuts, carry two epinephrine pens. Always. One might not work. Trust me.
Aboobakar Muhammedali
December 22, 2025 AT 00:32so many people dont understand this
i had a rash after amoxicillin when i was 12 and now at 34 i avoid all antibiotics
but last year i got pneumonia and they gave me azithromycin and i was fine
maybe i was never allergic maybe it was the virus
why dont doctors tell us this
why do we just live in fear
thank you for this post
Laura Hamill
December 23, 2025 AT 08:19THEY’RE LYING TO YOU. EVERY SINGLE TIME. THEY WANT YOU TO BE AFRAID OF PENICILLIN SO YOU’LL TAKE THE EXPENSIVE BRANDS. THEY’RE MAKING BILLIONS OFF YOUR FEAR. DID YOU KNOW THE FDA GOT PAID BY PHARMA TO PUSH THESE ‘ALLERGY’ LABELS? THEY DON’T WANT YOU TO KNOW YOU CAN BE TESTED. THEY WANT YOU TO STAY AFRAID. I’VE SEEN THE DOCUMENTS. THEY’RE HIDING THE TRUTH. YOU THINK YOU’RE ALLERGIC? YOU’RE JUST A PROFIT CENTER.
THEY ALSO MADE YOU THINK LACTOSE IS BAD. IT’S NOT. IT’S THE FILLER. THEY PUT CHEAP FILLERS IN PILLS TO MAKE MORE MONEY. YOU’RE ALLERGIC TO LACTOSE? NO. YOU’RE ALLERGIC TO CORPORATE GREED.
Alana Koerts
December 23, 2025 AT 08:38So you’re saying 90% of penicillin allergies are false? That’s a huge claim. Where’s the meta-analysis? The 2022 case study? That’s one woman with a lactose filler. That’s not a population trend. And you’re conflating intolerance with allergy. You’re oversimplifying T-cell mediated reactions. This reads like a press release, not medical advice.
Also - ‘component-resolved diagnostics’ isn’t FDA-approved for peanuts. It’s available in some labs. Don’t mislead people. You’re doing more harm than good.
William Liu
December 23, 2025 AT 23:07Thank you for this. I’ve been avoiding all NSAIDs since my 20s because of a rash after Advil. I never thought to ask if it was the aspirin or the dye. I’m going to book an appointment with my allergist. No more living in fear. Just because something happened once doesn’t mean it’ll happen again. I’m ready to find out what’s really going on.
Kinnaird Lynsey
December 25, 2025 AT 05:30…I’m not sure I believe the part about 90% of penicillin allergies being false. That feels… convenient. Like someone wants us to stop being cautious. But then again, I did get a rash after amoxicillin once and it was just a virus. So maybe? I don’t know. I’m just saying - I’d rather be safe than sorry. But also - maybe I’m being paranoid. I’ll think about it.
Anna Sedervay
December 26, 2025 AT 13:28It is profoundly concerning that the medical establishment continues to propagate such reductive diagnostic paradigms. The conflation of IgE-mediated responses with T-cell-driven hypersensitivities is not merely a clinical oversight - it is a systemic epistemological failure. One must interrogate the institutional incentives behind the perpetuation of the penicillin allergy mythos. Is it profit? Incompetence? Or the commodification of fear as a tool of pharmaceutical hegemony? I have reviewed the 2023 ImmunoCAP® data - it is statistically robust - yet still, the medical community resists paradigmatic shift. Why? Because to admit error is to invite liability. And liability, as we know, is monetized.
Matt Davies
December 26, 2025 AT 20:51Man, I used to think I was allergic to shellfish because I got a stomach ache after shrimp. Turns out I just ate it with a ton of garlic and butter. My body’s like ‘WHAT IS THIS SAVAGE COMBINATION?!’
But seriously - this post is a gift. I’m telling my sister. She’s been avoiding all dairy because she thinks she’s allergic. She’s just lactose intolerant. She’s been missing out on ice cream for 10 years. I’m sending her this with a 🍦 emoji. She’s gonna cry. And then eat a whole pint.
Mike Rengifo
December 28, 2025 AT 05:39So I got a rash after amoxicillin in college. Thought I was allergic. Never took it again. Last year I had strep, took it again, no problem. Guess I was just sick that time. Anyway - I’m gonna get tested. I’ve been avoiding penicillin for 12 years. That’s a lot of time spent being scared of a ghost.