When you pick up a generic pill from the pharmacy, you expect it to work just like the brand-name version. But behind that simple tablet is a complex manufacturing process-and one that’s far more prone to errors than most people realize. In 2023, generic drug defects led to over 1,800 adverse event reports to the FDA, with patients describing crumbling tablets, discolored pills, and unexpected side effects that didn’t match their previous prescriptions. These aren’t isolated mistakes. They’re symptoms of a broken system.
Why Generic Drugs Have More Quality Problems
Generic drugs make up 90% of prescriptions in the U.S., but they account for nearly two-thirds of all drug shortages. Why? Because the business model rewards low cost over high quality. Branded drug companies spend 15-18% of their production budget on quality control. Generic manufacturers, under intense price pressure, average just 8-10%. That gap shows up in the numbers: 57% of generic manufacturing facilities failed FDA inspections in recent years, compared to 28% for branded ones. The pressure to cut costs leads to shortcuts. Older equipment isn’t replaced. Staff training is reduced. Facilities that once made one type of drug now produce five or six, increasing the risk of cross-contamination. And when a company is competing on price alone, investing in real-time monitoring systems or automated visual inspection becomes a luxury-not a necessity.Common Defects You Might Not Notice (But Can Feel)
Not all defects are obvious. Some are invisible until they cause harm. Here are the most frequent manufacturing issues in generic drugs:- Capping: The top or bottom of a tablet splits off during handling. This happens when compression force exceeds 15 kN and the tablet’s moisture content is below 2%. It’s common in hydrophobic formulations like metformin ER. Patients report pills crumbling in their hands or the blister pack.
- Lamination: Layers of the tablet separate. This occurs at turret speeds over 40 rotations per minute when pre-compression is too weak. It’s especially dangerous in extended-release pills, where the inner layer might release all its drug at once.
- Weight variation: Tablets vary in weight by more than 5%. This is a major safety issue. If a tablet is too light, you’re not getting enough medicine. Too heavy, and you risk overdose. Granule flow rates below 0.5 g/s cause this in 12.7% of defective batches.
- Punch sticking: The active ingredient sticks to the machine’s punch head. This happens with APIs that melt below 120°C when moisture levels rise above 4%. The result? Inconsistent dosing-some pills are underdosed, others overdosed.
- Mottling: Uneven coloring. While mostly cosmetic, severe mottling can signal poor mixing of ingredients. In one 2023 case, patients taking a generic levothyroxine reported inconsistent energy levels, later traced to inconsistent API distribution due to mottling.
- Particulate contamination: Tiny particles in injectables. This is the #1 cause of sterile product recalls. A single speck of metal or glass in an IV bag can trigger a severe immune reaction.
How Defects Lead to Real-World Harm
A tablet that looks fine might still be dangerous. In 2021, a batch of generic metformin ER was recalled after pharmacists noticed tablets crumbling during dispensing. Patients reported nausea, diarrhea, and uncontrolled blood sugar-symptoms that didn’t match the brand version they’d used for years. Testing revealed the granules were too dry, causing poor binding. The batch had passed visual inspection. Sterile injectables are even riskier. In 2022, a generic heparin batch caused multiple hospital-acquired infections due to bacterial contamination from a poorly cleaned line. The facility had been producing multiple drugs on the same equipment without proper cleaning validation. Patient reports on Reddit and pharmacy forums are full of similar stories: “My generic thyroid pill made me shaky-switched back to brand and felt normal again.” “The new generic statin gave me muscle pain my old one never did.” These aren’t just placebo effects. Bioequivalence studies show 7.3% of generic applications between 2015 and 2020 failed due to manufacturing inconsistencies, not formulation differences.
Why the System Keeps Failing
Regulators know the problems exist. The FDA issued 42% of its 2023 Warning Letters to generic manufacturers for manufacturing defects. The European Medicines Agency saw a 29% to 37% rise in rejected certifications for generics between 2019 and 2023. Yet, the root causes remain unchanged. The biggest issue? Aging infrastructure. Many generic manufacturing plants in India and China were built in the 1990s. They still use batch processing-where each step is done in separate tanks-instead of continuous manufacturing, which is more precise and less prone to error. Continuous manufacturing reduces defect rates by 65%, but only 47 generic manufacturers have adopted it as of early 2024. Cost is the barrier. Upgrading a single production line can cost $10 million. The Generic Pharmaceutical Association estimates it would take $28.7 billion to modernize all U.S. generic facilities. Annual investment? Just $1.2 billion. That’s why the defect rate remains at 66,000 per million opportunities-far above the 3.4 per million standard in other industries.What’s Being Done-and What’s Not
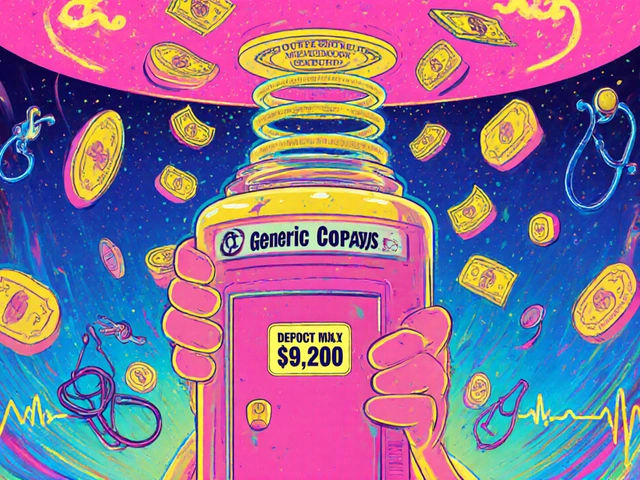
There are solutions, but adoption is slow. The FDA’s Quality by Design (QbD) guidelines require manufacturers to define a “design space” where critical parameters like temperature, pressure, and moisture are tightly controlled. But compliance is voluntary unless you’re applying for a new drug. Some companies are stepping up. Sandoz and Dr. Reddy’s are using AI-powered inspection systems that detect defects as small as 0.1 mm with 92% accuracy. Traditional human inspection misses 30% of flaws. These systems reject bad tablets at 600 per minute-far faster and more reliable. In-line weight monitoring is another win. Systems that check every tablet’s weight in real time and automatically reject those outside ±5% of target have cut batch failures by 40% in pilot programs. But only a handful of manufacturers use them. The 2024 Drug Supply Chain Security Act now requires track-and-trace for high-risk generics. Early results show a 22% drop in counterfeit-related issues. But counterfeit drugs are only a small part of the problem. The real issue is poor manufacturing-something the law doesn’t fix.
What You Can Do as a Patient
You can’t control the factory. But you can protect yourself:- Check your pills. If your generic looks different-color, shape, markings-ask your pharmacist. Don’t assume it’s the same.
- Report odd side effects. If your generic causes new symptoms, report it to the FDA’s MedWatch system. Your report adds to the data that drives recalls.
- Ask about the manufacturer. Some generic makers have far better records than others. Teva had a 0.8% batch rejection rate in 2023. Smaller firms averaged 3.2%.
- Stick with one brand if it works. If you’ve found a generic that works for you, don’t switch unless you have to. Switching between manufacturers can trigger unintended side effects.
- Know your options. For critical drugs like levothyroxine, warfarin, or seizure meds, your doctor can prescribe the brand if quality concerns arise. Insurance often covers it if you document the issue.






Gerard Jordan
January 19, 2026 AT 13:32Man, I had no idea pills could just fall apart in my hand 😱 I switched to a generic metformin last year and thought my stomach issues were just 'new normal'-turns out the tablet was crumbling. Took me 3 months to figure it out. Now I check every pill like it’s a diamond. 🤯
michelle Brownsea
January 20, 2026 AT 09:14Let me be perfectly clear: this isn't a 'manufacturing defect'-it's a systemic betrayal of public trust! The FDA, the pharmaceutical industry, and every politician who voted against mandatory quality standards are complicit in this slow-motion public health crisis! Where is the outrage?! Where is the accountability?! This isn't just negligence-it's criminal! And don't even get me started on the fact that people are dying because of substandard pills that cost $0.12 to produce! 🤬
Melanie Pearson
January 22, 2026 AT 07:05It is not surprising that the United States has become a global leader in pharmaceutical mediocrity. The prioritization of cost-efficiency over patient safety is a direct consequence of deregulatory policies enacted over the past three decades. The fact that 57% of generic manufacturing facilities fail inspection is not an anomaly-it is the logical endpoint of market-driven healthcare. The Department of Health and Human Services must institute mandatory, real-time quality monitoring with independent third-party auditing. Failure to do so constitutes a dereliction of duty.
Uju Megafu
January 23, 2026 AT 15:57Oh my GOD. I’ve been taking this generic thyroid med for 2 years and I’ve been so tired, my hair’s falling out, I cry for no reason-I thought it was menopause! Then I switched back to brand and BOOM-like I got my life back. I posted about it on Instagram and 12 women DM’d me saying the same thing. This is a MASSIVE cover-up. Who’s paying off the FDA??
Jarrod Flesch
January 25, 2026 AT 10:36Been a pharmacist in Melbourne for 18 years. Saw this coming. The worst part? Most patients don’t even know their pills changed. They just feel ‘off’ and blame themselves. I keep a little cheat sheet of which generics are actually reliable-Teva, Sandoz, Mylan (before the mess). If you’re on something critical-thyroid, seizure meds, blood thinners-ask for the manufacturer. It’s your right. And if your pharmacist looks confused? Walk out. 😌
Kelly McRainey Moore
January 25, 2026 AT 13:48I just checked my levothyroxine bottle-yep, different color than last month. Didn’t think much of it. Now I’m gonna call my pharmacy tomorrow. Thanks for the heads-up, this is super helpful. 😊
Stephen Rock
January 26, 2026 AT 22:02People pay $200 for brand name pills and cry when generics cost $4. You get what you pay for. If you want quality, pay for it. Stop pretending you’re saving money when you’re just gambling with your life.
Ashok Sakra
January 26, 2026 AT 23:02India make good medicine! Why you say bad? My cousin take generic from India, no problem! You American scare easy. We make 80% world medicine. You don’t know how it made. You just complain. I work in factory, we check every pill. You don’t believe me? I show you video!
Andrew Rinaldi
January 27, 2026 AT 23:24It’s hard to reconcile the fact that we live in a world where a life-saving pill can be made in a 30-year-old factory with outdated machinery, and yet we still expect it to be safe. Maybe the real question isn’t why these defects happen-but why we’ve accepted them as normal. We’ve normalized risk in healthcare because we’re afraid to pay more. But what’s the cost of a life? Maybe it’s time we stopped pretending this is just a manufacturing issue. It’s a moral one.